Independent and joint associations of hypertension and depression with cardiovascular diseases and all-cause mortality: a population-based cohort study
IF 3.4
4区 医学
Q2 PERIPHERAL VASCULAR DISEASE
引用次数: 0
Abstract
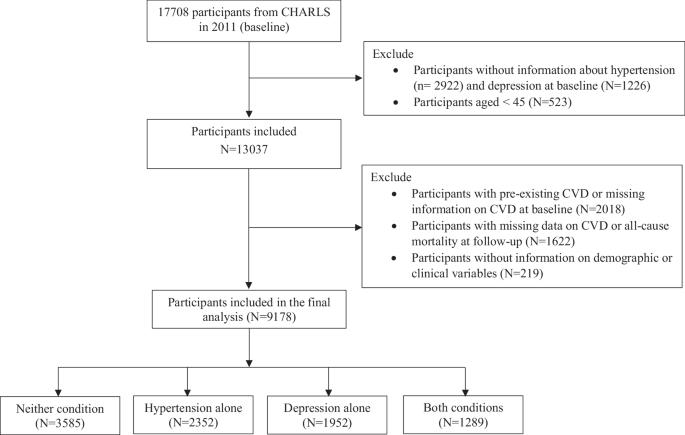
Hypertension frequently co-exists with depression, leading to adverse health outcomes. This study aimed to examine the individual and joint effects of hypertension and depression on the risks of new-onset cardiovascular disease (CVD) and all-cause mortality among the middle-aged and older Chinese individuals. Data from the China Health and Retirement Longitudinal Study (CHARLS) during 2011–2020 were used. Participants were divided into four groups for comparison: hypertension alone, depression alone, both conditions, neither condition. Multivariate logistic regression models were established to compare the risks of all-cause mortality and CVD among the four groups. A total of 9178 participants without pre-existing CVD were included and followed for nine years. Compared with individuals with neither condition, the risk of all-cause mortality increased among individuals with hypertension alone (adjusted odds ratio [aOR]: 1.414, 95% confidence interval [CI]: 1.133–1.764), depression alone (aOR: 1.023, 95% CI: 0.795–1.317) and comorbid hypertension and depression (aOR: 1.524, 95% CI: 1.180–1.968). The aORs for CVD events in individuals with both conditions, hypertension alone, and depression only were 2.207 (95% CI: 1.885–2.584), 1.945 (95% CI: 1.702–2.222) and 1.572 (95% CI: 1.365–1.809), respectively. Furthermore, those with severe depressive symptoms were at higher risks of all-cause mortality and CVD, regardless of having hypertension. Hypertension with comorbid depression leads to higher risks of CVD and all-cause mortality than either condition alone. Screening and management of depression among individuals with hypertension are essential for the primary prevention of CVD and premature death.
高血压和抑郁症与心血管疾病和全因死亡率的独立和联合关联:一项基于人群的队列研究
高血压经常与抑郁症共存,导致不良的健康结果。本研究旨在探讨高血压和抑郁对中国中老年人群新发心血管疾病(CVD)风险和全因死亡率的个体和联合影响。数据来自2011-2020年中国健康与退休纵向研究(CHARLS)。参与者被分成四组进行比较:单独高血压、单独抑郁、两种情况都有、两种情况都没有。建立多因素logistic回归模型,比较四组患者的全因死亡率和心血管疾病风险。共有9178名没有既往心血管疾病的参与者被纳入研究,随访9年。与无上述两种疾病的患者相比,单独高血压患者(校正优势比[aOR]: 1.414, 95%可信区间[CI]: 1.133-1.764)、单独抑郁患者(aOR: 1.023, 95% CI: 0.795-1.317)和合并高血压和抑郁患者(aOR: 1.524, 95% CI: 1.180-1.968)的全因死亡风险增加。合并高血压和抑郁症的CVD事件的aor分别为2.207 (95% CI: 1.885-2.584)、1.945 (95% CI: 1.702-2.222)和1.572 (95% CI: 1.365-1.809)。此外,那些有严重抑郁症状的人患全因死亡率和心血管疾病的风险更高,无论是否患有高血压。高血压合并抑郁症导致心血管疾病和全因死亡率的风险高于单独的任何一种情况。高血压患者抑郁症的筛查和管理对于心血管疾病和过早死亡的一级预防至关重要。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Human Hypertension
医学-外周血管病
CiteScore
5.20
自引率
3.70%
发文量
126
审稿时长
6-12 weeks
期刊介绍:
Journal of Human Hypertension is published monthly and is of interest to health care professionals who deal with hypertension (specialists, internists, primary care physicians) and public health workers. We believe that our patients benefit from robust scientific data that are based on well conducted clinical trials. We also believe that basic sciences are the foundations on which we build our knowledge of clinical conditions and their management. Towards this end, although we are primarily a clinical based journal, we also welcome suitable basic sciences studies that promote our understanding of human hypertension.
The journal aims to perform the dual role of increasing knowledge in the field of high blood pressure as well as improving the standard of care of patients. The editors will consider for publication all suitable papers dealing directly or indirectly with clinical aspects of hypertension, including but not limited to epidemiology, pathophysiology, therapeutics and basic sciences involving human subjects or tissues. We also consider papers from all specialties such as ophthalmology, cardiology, nephrology, obstetrics and stroke medicine that deal with the various aspects of hypertension and its complications.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


