Variation in Students' Experiences and Approaches to Learning During Early Clinical Immersion
Abstract
Introduction
Emphasis is being placed on producing intern-ready graduates who can navigate complex clinical environments. Early clinical immersion seeks to enable this through experiential learning and supported participation in authentic workplaces; however, its educational value remains intangible. Studies have evaluated placement objectives but not other effects in detail. We explored novice students' experiences and approaches to learning during early clinical immersion and factors that enhanced or hindered them.
Methods
Medical students at the beginning of their second year undertook 8 weeks of immersive clinical learning to introduce them to hospital settings, enable understanding of hospital workplaces and strengthen clinical assessment and skills. In 2021, focus groups were conducted and data were analysed using theory-informing subjectivist inductive data analysis based on self-regulation learning theory.
Results
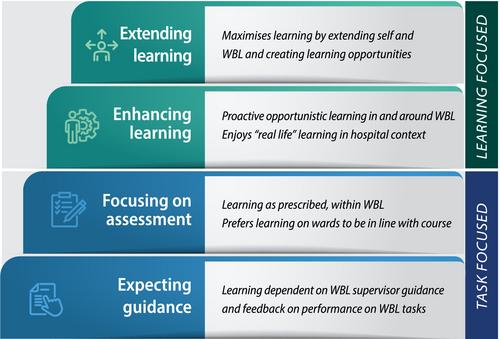
Fifteen participants described diverse experiences and approaches to learning during early clinical immersion, indicating varying degrees of self-regulated learning. Through goal setting, strategic awareness and behaviour, self-reflection and adaptation and flexibility, some maximised learning opportunities, while others had a more limited experience. Some causal attributes enhanced learning, such as undertaking ward-based learning tasks with nurses, while other attributes hindered it, such as disengaged supervisors and teams.
Conclusions
The quality of students' experience of learning during early clinical immersion is influenced by the degree of self-regulated learning, which affects the approach to learning, plus system barriers and facilitators. Strategies that enable students to enhance self-regulated learning, such as setting and monitoring learning goals with supervisors, may help optimise learning in clinical environments and provide the scaffolds to enhance learning.




 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


