Safety and Effectiveness of Image-Guided Therapies for Giant Hepatic Hemangiomas: A Systematic Review and Meta-Analysis of 2,617 Patients
IF 2.6
3区 医学
Q2 PERIPHERAL VASCULAR DISEASE
Journal of Vascular and Interventional Radiology
Pub Date : 2025-07-07
DOI:10.1016/j.jvir.2025.06.025
引用次数: 0
Abstract
Purpose
To evaluate the safety and effectiveness of image-guided therapies—including transarterial chemoembolization (TACE), radiofrequency (RF) ablation, microwave ablation, and percutaneous sclerotherapy—for the treatment of giant hepatic hemangiomas (GHHs).
Materials and Methods
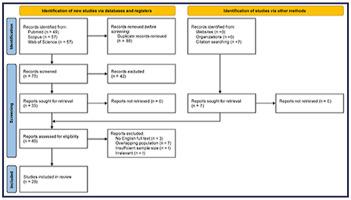
A comprehensive search was performed across PubMed, Scopus, and Web of Science, including studies with ≥5 patients that reported image-guided treatment of GHHs. Primary outcomes included technical success, adverse events (AEs; classified according to the Society of Interventional Radiology [SIR] system), clinical success (symptom relief without additional intervention), and radiologic success (≥50% size reduction and/or lack of enhancement on follow-up imaging). A subgroup analysis was performed for GHHs of ≥10 cm. Outcomes were analyzed using a random-effect meta-analysis.
Results
Twenty-eight studies (2,617 patients; 32.5% men; mean age, 46.1 years [SD ± 3.2]) with 2,996 GHHs, ranging from 4 to 30 cm, were included. Of these, 22 were noncomparative, and 6 compared either 2 image-guided therapies or surgery, reporting outcomes for TACE (n = 13), RF ablation (n = 7), microwave ablation (n = 6), and percutaneous sclerotherapy (n = 4). The pooled technical success rate was 99.9%. Grade 2–4 AEs occurred in 1.64%, with TACE having the lowest rate (0.2%) and RF ablation the highest (2.1%). Clinical success at final follow-up was 99.9%, while radiological success was 85.7%. Grade 2–4 AEs were significantly higher in the subanalysis of GHHs of ≥10 cm (10.6%; P < .001), despite similar technical success and radiological and clinical outcomes.
Conclusions
Image-guided therapies are safe and effective for GHHs, achieving high technical, clinical, and radiological success with minimal Grade 2–4 AEs. However, for GHHs ≥10 cm, AE rates were higher.
图像引导治疗巨大肝血管瘤的安全性和有效性:2617例患者的系统回顾和荟萃分析
目的:评价图像引导治疗(包括经动脉化疗栓塞(TACE)、射频消融(RFA)、微波消融(MWA)和经皮硬化治疗(PS))治疗巨大肝血管瘤(GHHs)的安全性和有效性。材料和方法:在PubMed、Scopus和Web of Science上进行了全面的搜索,包括有≥5例患者报告图像引导治疗GHHs的研究。主要结局包括技术成功、不良事件(AE;根据介入放射学会系统分类),临床成功(症状缓解,无需额外干预)和放射学成功(≥50%的尺寸缩小和/或随访成像缺乏增强)。GHHs≥10 cm进行亚组分析。结果分析采用随机效应荟萃分析。结果:28项研究(2617例患者;男性32.5%;平均年龄:46.1±3.2岁),ghh 2996例,身高4 ~ 30 cm。其中,22例为非对比性,6例为两种图像引导疗法或手术的比较,报告了TACE (n = 13)、RFA (n = 7)、MWA (n = 6)和PS (n = 4)的结果。综合技术成功率为99.9%。2-4级ae发生率为1.64%,其中TACE发生率最低(0.2%),RFA发生率最高(2.1%)。最终随访临床成功率为99.9%,放射学成功率为85.7%。GHHs≥10 cm亚分析中,2-4级ae显著升高(10.6%;P < 0.001),尽管技术成功,放射学和临床结果相似。结论:图像引导治疗GHHs是安全有效的,在技术、临床和放射学上都取得了很高的成功,2-4级ae最小。但GHHs≥10 cm时,AE发生率较高。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
4.30
自引率
10.30%
发文量
942
审稿时长
90 days
期刊介绍:
JVIR, published continuously since 1990, is an international, monthly peer-reviewed interventional radiology journal. As the official journal of the Society of Interventional Radiology, JVIR is the peer-reviewed journal of choice for interventional radiologists, radiologists, cardiologists, vascular surgeons, neurosurgeons, and other clinicians who seek current and reliable information on every aspect of vascular and interventional radiology. Each issue of JVIR covers critical and cutting-edge medical minimally invasive, clinical, basic research, radiological, pathological, and socioeconomic issues of importance to the field.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


