Platelets as drivers of immunothrombosis in rheumatic diseases
IF 32.7
1区 医学
Q1 RHEUMATOLOGY
引用次数: 0
Abstract
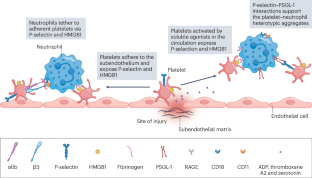
Platelets are central players in inflammatory and thrombotic responses that drive the onset and progression of rheumatic diseases. In particular, they regulate immunothrombosis, a defence mechanism in which the immune and blood-clotting systems cooperate to contain infections or vascular damage. Although immunothrombosis can help to preserve blood-vessel integrity and promote healing, it becomes harmful when exaggerated or chronic. In rheumatic diseases, such as systemic lupus erythematosus, systemic sclerosis and antiphospholipid syndrome, immunothrombosis contributes to persistent inflammation, abnormal blood-clot formation and long-term damage to the small blood vessels. It has also been implicated in maintaining autoimmune responses to autoantigens released by neutrophils. Platelets are among the first responders to vascular injury and influence the activity of immune cells, particularly neutrophils, by promoting the formation of neutrophil extracellular traps. Platelets express proteins such as P-selectin and the damage-associated molecule high-mobility group box 1 (HMGB1), which have distinct and non-redundant roles, both via direct interactions locally at sites of vascular damage and systemically via the release of extracellular vesicles. Understanding how platelets contribute to vascular inflammation and clotting in autoimmune settings elucidates disease mechanisms and might lead to the identification of new therapeutic targets. This Review provides an overview of how platelets promote immunothrombosis in rheumatic disease. The authors discuss the different ways in which platelets and immunothrombosis can be targeted for therapeutic intervention.

血小板作为风湿病免疫血栓形成的驱动因素
血小板是炎症和血栓形成反应的核心参与者,这些反应驱动风湿病的发生和进展。特别是,它们调节免疫血栓形成,这是一种免疫和凝血系统合作抑制感染或血管损伤的防御机制。虽然免疫血栓可以帮助保持血管的完整性和促进愈合,但当它被夸大或慢性时就会变得有害。在风湿性疾病中,如系统性红斑狼疮、系统性硬化症和抗磷脂综合征,免疫血栓形成导致持续炎症、异常血凝块形成和对小血管的长期损害。它还涉及维持对中性粒细胞释放的自身抗原的自身免疫反应。血小板是血管损伤的第一反应者之一,通过促进中性粒细胞胞外陷阱的形成,影响免疫细胞,特别是中性粒细胞的活性。血小板表达p -选择素和损伤相关分子高迁移率组盒1 (HMGB1)等蛋白,它们通过血管损伤部位的局部直接相互作用和通过细胞外囊泡的系统性释放,发挥着独特而非冗余的作用。了解血小板如何在自身免疫环境下促进血管炎症和凝血,阐明疾病机制,并可能导致新的治疗靶点的确定。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Nature Reviews Rheumatology
医学-风湿病学
CiteScore
29.90
自引率
0.90%
发文量
137
审稿时长
6-12 weeks
期刊介绍:
Nature Reviews Rheumatology is part of the Nature Reviews portfolio of journals. The journal scope covers the entire spectrum of rheumatology research. We ensure that our articles are accessible to the widest possible audience.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


