Thermal Ablation Modalities That Best Compete with Partial Nephrectomy for T1A and T1B Renal Cell Carcinoma: A Network Meta-Analysis
IF 2.6
3区 医学
Q2 PERIPHERAL VASCULAR DISEASE
Journal of Vascular and Interventional Radiology
Pub Date : 2025-07-04
DOI:10.1016/j.jvir.2025.05.032
引用次数: 0
Abstract
Purpose
To address the lack of consensus on the ranking of thermal ablation (TA) for treating T1A and T1B renal cell carcinoma (RCC), a network meta-analysis was conducted to compare the efficacy and safety of different TA modalities for managing early-stage RCC.
Methods
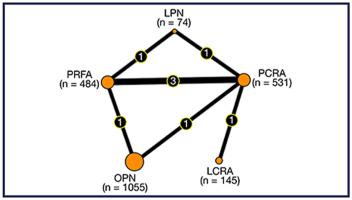
The Cochrane Library, PubMed, Scopus, and Web of Science were systematically searched for studies comparing percutaneous and laparoscopic radiofrequency ablation (RFA), cryoablation (CRA), and microwave ablation (MWA) with open, laparoscopic, and robotic partial nephrectomy (PN) for T1A and T1B RCC. Primary outcomes were recurrence-free survival (RFS), local recurrence, and postprocedural adverse events. Secondary outcomes included overall survival, cancer-specific mortality, changes in estimated glomerular filtration rate, hospital stay length, major adverse events, operation time, and systemic recurrence.
Results
Thirty-two studies were included, comprising 8,568 patients in T1A studies and 1,019 in T1B studies. For T1A tumors, no significant differences in 5-year RFS were observed between open PN and percutaneous RFA (P = .655), percutaneous CRA (P = .369), laparoscopic RFA (P = 1.000), or laparoscopic CRA (P = .547). However, percutaneous MWA reduced local recurrence (P = .033) and had lower postprocedural adverse events compared with PN (P = .029). For T1B tumors, no significant differences in 5-year RFS, local recurrence, or postprocedural adverse events were observed between open PN and percutaneous RFA or percutaneous CRA.
Conclusion
Although data gaps exist, percutaneous TA demonstrated outcomes comparable with surgery for both T1A and T1B renal tumors. For T1A tumors, percutaneous MWA may be highly effective. For T1B tumors, the similar outcomes across percutaneous approaches support tailoring treatment based on patient factors and operator expertise.
热消融治疗T1A和T1B肾细胞癌的最佳竞争方式:网络荟萃分析
背景:热消融(TA)治疗T1A和T1B肾细胞癌(RCC)的排名尚未达成共识。网络荟萃分析比较TA治疗T1A和T1B RCC的疗效和安全性。方法:系统检索Cochrane图书馆、PubMed、Scopus和Web of Science,比较经皮和腹腔镜射频消融(RFA)、冷冻消融(CRA)和微波消融(MWA)与开放、腹腔镜和机器人PN治疗T1A和T1B RCC的研究。主要结局是无复发生存(RFS)、局部复发和术后不良事件。次要结局包括总生存、癌症特异性死亡率、eGFR变化、住院时间、主要不良事件、手术时间和全身复发。结果:纳入32项研究,包括T1A研究8,568例患者和T1B研究1,019例患者。对于T1A肿瘤,开放PN与经皮RFA (P=0.655)、经皮CRA (P=0.369)、腹腔镜RFA (P=1.000)、腹腔镜CRA (P=0.547)的5年RFS无显著差异。然而,与PN相比,经皮MWA减少了局部复发(P=0.033),术后不良事件发生率更低(P=0.029)。对于T1B肿瘤,开放PN与经皮RFA或经皮CRA在5年RFS、局部复发或术后不良事件方面无显著差异。结论:尽管存在数据缺口,经皮TA治疗T1A和T1B肾肿瘤的结果与手术相当。对于T1A肿瘤,经皮MWA可能非常有效。对于T1B肿瘤,经皮入路的相似结果支持基于患者因素和操作人员专业知识的定制治疗。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
4.30
自引率
10.30%
发文量
942
审稿时长
90 days
期刊介绍:
JVIR, published continuously since 1990, is an international, monthly peer-reviewed interventional radiology journal. As the official journal of the Society of Interventional Radiology, JVIR is the peer-reviewed journal of choice for interventional radiologists, radiologists, cardiologists, vascular surgeons, neurosurgeons, and other clinicians who seek current and reliable information on every aspect of vascular and interventional radiology. Each issue of JVIR covers critical and cutting-edge medical minimally invasive, clinical, basic research, radiological, pathological, and socioeconomic issues of importance to the field.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


