Impact of diabetes on three-year outcome after coronary stenting in patients with polyvascular atherosclerotic disease – a secondary analysis of the randomized TWENTE trials
IF 2.5
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
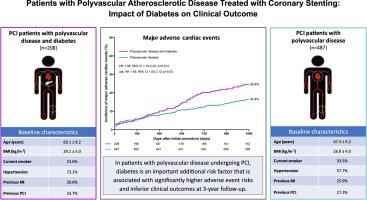
The presence of polyvascular atherosclerotic disease is associated with a high-risk of adverse events following percutaneous coronary intervention (PCI). As the extent to which the presence of diabetes further increases this elevated risk is unclear, based on current literature, we sought to assess the long-term outcome after PCI in patients with polyvascular disease, comparing those with and without diabetes.
Methods
The current study population consists of patients with known polyvascular disease, identified from a pooled patient-level database of 4 PCI trials in all-comers treated with new-generation drug-eluting stents; no exclusion criteria were set. The main composite endpoint was major adverse cardiac event (MACE: any myocardial infarction, emergent coronary bypass surgery, clinically indicated target lesion revascularization, or all-cause mortality).
Results
695 patients had polyvascular disease of whom 208(29.9 %) had diabetes. Patients with diabetes were older, had a higher body-mass-index, and had a higher prevalence of hypertension than those without diabetes. At 3-year follow-up, the incidence of MACE was significantly higher in polyvascular disease patients with diabetes (24.6 % vs.16.4 %, adj.HR:1.49, 95 %CI:1.05–2.12, p = 0.03), in particular insulin-treated patients, and was primarily attributable to a disparity in all-cause mortality which was more than twice as high in patients with diabetes (15.4 % vs.7.2 %, p < 0.001). Furthermore, the risk of repeated target vessel revascularization was higher in patients with diabetes (12.0 % vs7.0 %, adj.HR:1.88, 95 %CI:1.12–3.16, p = 0.02).
Conclusions
In the high-risk population of PCI patients with polyvascular disease, the presence of diabetes represents a profoundly significant additional risk factor at long-term follow-up, associated with significantly higher adverse event risks.
Trial registration: ClinicalTrials.gov NCT01066650 NCT0133170 NCT01674803 NCT02508714.
糖尿病对多血管粥样硬化性疾病患者冠状动脉支架植入术后3年预后的影响——对随机TWENTE试验的二次分析
背景:多血管粥样硬化性疾病的存在与经皮冠状动脉介入治疗(PCI)后不良事件的高风险相关。由于糖尿病的存在在多大程度上进一步增加这种风险尚不清楚,基于现有文献,我们试图评估多血管疾病患者PCI后的长期结果,比较有糖尿病和无糖尿病患者。方法:目前的研究人群包括已知的多血管疾病患者,从4项PCI试验的合并患者水平数据库中确定,这些患者接受新一代药物洗脱支架治疗;未设置排除标准。主要的复合终点是主要的心脏不良事件(MACE:任何心肌梗死、紧急冠状动脉搭桥手术、临床指示的靶病变血运重建术或全因死亡率)。结果695例患者合并多血管疾病,其中糖尿病208例(29.9%)。糖尿病患者年龄较大,身体质量指数较高,高血压患病率高于非糖尿病患者。在3年的随访中,多血管疾病合并糖尿病患者的MACE发生率明显更高(24.6% vs. 16.4%, hr:1.49, 95% CI: 1.05-2.12, p = 0.03),特别是胰岛素治疗的患者,这主要是由于糖尿病患者的全因死亡率差异(15.4% vs. 7.2%, p <;0.001)。此外,糖尿病患者发生反复靶血管重建术的风险更高(12.0% vs 7.0%,相对危险度:1.88,95% CI: 1.12-3.16, p = 0.02)。结论在PCI合并多血管疾病的高危人群中,糖尿病的存在在长期随访中是一个非常重要的额外危险因素,与明显较高的不良事件风险相关。试验注册:ClinicalTrials.gov NCT01066650 NCT0133170 NCT01674803 NCT02508714。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

IJC Heart and Vasculature
Medicine-Cardiology and Cardiovascular Medicine
CiteScore
4.90
自引率
10.30%
发文量
216
审稿时长
56 days
期刊介绍:
IJC Heart & Vasculature is an online-only, open-access journal dedicated to publishing original articles and reviews (also Editorials and Letters to the Editor) which report on structural and functional cardiovascular pathology, with an emphasis on imaging and disease pathophysiology. Articles must be authentic, educational, clinically relevant, and original in their content and scientific approach. IJC Heart & Vasculature requires the highest standards of scientific integrity in order to promote reliable, reproducible and verifiable research findings. All authors are advised to consult the Principles of Ethical Publishing in the International Journal of Cardiology before submitting a manuscript. Submission of a manuscript to this journal gives the publisher the right to publish that paper if it is accepted. Manuscripts may be edited to improve clarity and expression.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


