Redo surgical aortic valve replacement: An outdated technique in the era of valve-in-valve procedures?
IF 2.2
3区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
The treatment of degenerative prosthetic aortic valves is increasingly important. However, redo surgical aortic valve replacement (Re-SAVR) carries higher perioperative risks than primary surgical aortic valve replacement.
Aim
This study aims to identify predictors of early morbidity and death after Re-SAVR.
Methods
A retrospective analysis of 220 patients scheduled for elective Re-SAVR between 2009 and 2017 was conducted. Patients were divided into isolated (n = 87) and combined (n = 133) redo procedures. The primary endpoint was in-hospital death, and secondary endpoints were postoperative complications, such as stroke, dialysis and pacemaker implantation. Regression analysis identified independent predictors of death.
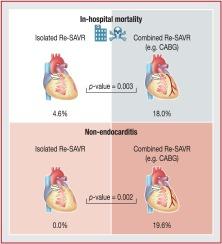
Results
Among the patients undergoing Re-SAVR (mean age, 62.6 ± 13.2 years; 71% male; mean EuroSCORE II, 12.6 ± 11.1%), 86.4% received biological prostheses and 13.6% received mechanical prostheses. The in-hospital death rate was 5.7% for isolated Re-SAVR and 18.0% for combined procedures (P = 0.003). Excluding patients with endocarditis, the in-hospital death rate was 0% for isolated Re-SAVR and 19.7% for combined procedures (P = 0.002). The incidence of postoperative complications after an isolated procedure was similar to that after a combined procedure. Independent predictors of 30-day death were previous coronary artery bypass grafting (odds ratio: 14.12, 95% confidence interval: 4.40–51.35; P < 0.001), a combined procedure (odds ratio: 7.01, 95% confidence interval: 2.09–31.54; P = 0.004) and New York Heart Association functional class III/IV (odds ratio: 3.73, 95% confidence interval: 1.31–12.58; P = 0.020).
Conclusions
The perioperative risk of death after isolated Re-SAVR in patients without endocarditis was 0%. Independent predictors of in-hospital death included previous coronary artery bypass grafting, combined procedures and New York Heart Association class III/IV. These findings may inform the decision-making process of the heart team regarding the optimal approach (surgical or transcatheter) for redo aortic valve replacement.
重做主动脉瓣置换术:在瓣中瓣手术时代是一种过时的技术吗?
背景:退行性人工主动脉瓣的治疗越来越重要。然而,重做手术主动脉瓣置换术(Re-SAVR)比初次手术主动脉瓣置换术有更高的围手术期风险。目的:本研究旨在确定Re-SAVR术后早期发病和死亡的预测因素。方法:回顾性分析2009年至2017年220例计划择期Re-SAVR的患者。患者分为单独(n=87)和联合(n=133)重做手术。主要终点是院内死亡,次要终点是术后并发症,如中风、透析和起搏器植入。回归分析确定了独立的死亡预测因素。结果:接受Re-SAVR的患者(平均年龄62.6±13.2岁;男性71%;平均EuroSCORE II(12.6±11.1%),86.4%接受生物假体,13.6%接受机械假体。单独Re-SAVR的住院死亡率为5.7%,联合手术的住院死亡率为18.0% (P=0.003)。排除心内膜炎患者,单独Re-SAVR的住院死亡率为0%,联合手术的住院死亡率为19.7% (P=0.002)。单独手术后并发症的发生率与联合手术后相似。30天死亡的独立预测因素是既往冠状动脉搭桥术(优势比:14.12,95%可信区间:4.40-51.35;结论:无心内膜炎患者孤立性Re-SAVR围手术期死亡风险为0%。院内死亡的独立预测因素包括既往冠状动脉搭桥术、联合手术和纽约心脏协会III/IV级。这些发现可能会为心脏团队决定重做主动脉瓣置换术的最佳方法(手术或经导管)提供信息。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Archives of Cardiovascular Diseases
医学-心血管系统
CiteScore
4.40
自引率
6.70%
发文量
87
审稿时长
34 days
期刊介绍:
The Journal publishes original peer-reviewed clinical and research articles, epidemiological studies, new methodological clinical approaches, review articles and editorials. Topics covered include coronary artery and valve diseases, interventional and pediatric cardiology, cardiovascular surgery, cardiomyopathy and heart failure, arrhythmias and stimulation, cardiovascular imaging, vascular medicine and hypertension, epidemiology and risk factors, and large multicenter studies. Archives of Cardiovascular Diseases also publishes abstracts of papers presented at the annual sessions of the Journées Européennes de la Société Française de Cardiologie and the guidelines edited by the French Society of Cardiology.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


