Endoscopic Ultrasound-guided Drainage With Lumen-apposing Metal Stent versus Plastic Stent for the Treatment of Pancreatic Pseudocyst: A Systematic Review and Meta-analysis
Abstract
Background
Pancreatic pseudocyst (PP), following acute or chronic pancreatitis, may become symptomatic or persist beyond 6–8 weeks, requiring drainage. Endoscopic ultrasonography-guided drainage (EUS-D) is the preferred method, using double pigtail plastic stents (DPPS) or self-expandable metallic stents (SEMS), such as lumen-apposing metal stents (LAMS). This meta-analysis compares DPPS and LAMS in EUS-D for PP, focusing on technical success, clinical success, adverse events (AEs), recurrence, and procedure time.
Methods
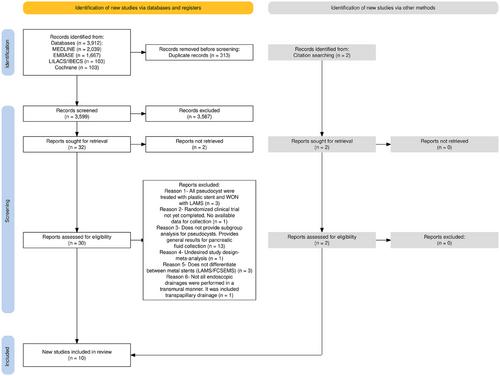
A search strategy was conducted in MEDLINE, Embase, Lilacs, and Cochrane databases according to PRISMA guidelines. Random-effect models were used for statistical analysis based on intention-to-treat. Heterogeneity was assessed using the I2 test. The risk of bias was assessed using the Risk of Bias in Non-randomized Studies—of Exposures tool. The quality of evidence was assessed using the Grading of Recommendations Assessment, Development, and Evaluation Tool.
Results
Ten studies were included: one prospective cohort and nine retrospective cohorts, conducted between 2014 and 2024. A total of 502 patients with PP were treated with EUS-D. The clinical success rate was higher using LAMS (Risk ratio [RR] = 1.05; 95% confidence interval [CI]: 1.01; 1.09; I2 = 0%), with shorter procedure time (Mean difference = -16.30; 95% CI: -27.65; -4.94; I2 = 86%) compared to DPPS. No statistical difference was observed for early and late AEs, recurrence, or technical success.
Conclusion
The study demonstrated that LAMS has a higher clinical success rate and a shorter procedure time compared to DPPS. There is no difference in terms of early and late AEs, recurrence, and technical success.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


