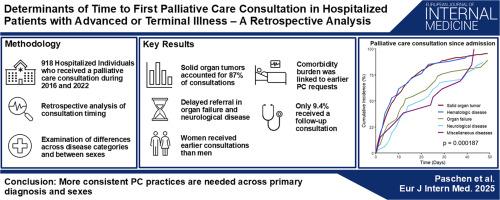
Determinants of time to first palliative care consultation in hospitalized patients with advanced or terminal illness – A retrospective analysis
IF 6.1
2区 医学
Q1 MEDICINE, GENERAL & INTERNAL
引用次数: 0
Abstract
Background
Diagnosis and sex-related biases can affect clinical decision-making in serious illness, including the recognition of palliative needs. Such biases may influence when and how patients receive palliative care (PC). This study aimed to investigate differences in timing and frequency of PC consultations by diagnosis, comorbidities, age, and sex among hospitalized patients.
Methods
This study retrospectively analyzed 918 patients (50.5 % female) who received a PC consultation during hospitalization between 2016 and 2022. Time from admission to first PC consultation was analyzed using a Cox proportional hazards model adjusted for primary diagnosis, comorbidities, age, and sex. Further analysis included number of follow-up consultations, time from primary disease onset to first PC consultation, and from consultation to discharge or death.
Results
Inpatients with organ failure (HR: 0.7 [95 %-CI: 0.5–0.9]; p = 0.02) or neurological diseases (HR: 0.7 [95 %-CI: 0.5–1.0]; p = 0.03) received later PC consultations than those with solid organ tumors or hematologic malignancies. Higher comorbidity burden was associated with earlier PC consultation (HR: 1.04 [CI: 1.01–1.07]; p = 0.02), while age was not linked to consultation timing (HR: 0.997 [CI: 0.992–1.002]; p = 0.20). Women received earlier PC consultations than men (HR: 1.3 [95 %-CI: 1.1–1.4]; p < 0.001). Only 9.4 % of individuals received a follow-up consultation, with the lowest proportion in subjects with organ failure (4.7 %).
Conclusions
This study highlights earlier PC consultation requests during hospitalization for individuals with malignant diseases and for women. The low rate of follow-up PC consultations indicates that the importance of regular PC involvement to improve patient’s outcomes still did not permeate into clinical practice.
晚期或绝症住院患者首次姑息治疗咨询时间的决定因素-回顾性分析。
背景:诊断和性别相关的偏见可以影响严重疾病的临床决策,包括对姑息治疗需求的认识。这种偏见可能会影响患者何时以及如何接受姑息治疗(PC)。本研究旨在探讨住院患者在诊断、合并症、年龄和性别方面PC会诊时间和频率的差异。方法:本研究回顾性分析2016年至2022年住院期间接受PC会诊的918例患者(50.5%为女性)。采用Cox比例风险模型对原发性诊断、合并症、年龄和性别进行调整,分析从入院到首次PC会诊的时间。进一步的分析包括随访会诊的次数、从原发性疾病发病到首次PC会诊的时间、从会诊到出院或死亡的时间。结果:住院患者发生器官衰竭(HR: 0.7 [95% -CI: 0.5-0.9];p = 0.02)或神经系统疾病(HR: 0.7 [95% -CI: 0.5-1.0];p = 0.03)比实体器官肿瘤或血液恶性肿瘤患者更晚接受PC咨询。较高的合并症负担与早期PC咨询相关(HR: 1.04 [CI: 1.01-1.07];p = 0.02),而年龄与咨询时间无关(HR: 0.997 [CI: 0.992-1.002];P = 0.20)。女性比男性更早接受PC咨询(HR: 1.3 [95% -CI: 1.1-1.4];P < 0.001)。只有9.4%的人接受了随访咨询,器官衰竭患者的比例最低(4.7%)。结论:本研究强调了恶性疾病患者和妇女住院期间早期PC咨询请求。PC的低随访率表明定期PC介入对改善患者预后的重要性仍未渗透到临床实践中。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
9.60
自引率
6.20%
发文量
364
审稿时长
20 days
期刊介绍:
The European Journal of Internal Medicine serves as the official journal of the European Federation of Internal Medicine and is the primary scientific reference for European academic and non-academic internists. It is dedicated to advancing science and practice in internal medicine across Europe. The journal publishes original articles, editorials, reviews, internal medicine flashcards, and other relevant information in the field. Both translational medicine and clinical studies are emphasized. EJIM aspires to be a leading platform for excellent clinical studies, with a focus on enhancing the quality of healthcare in European hospitals.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


