Hypertensive urgencies and emergencies in the cardiology emergency department: epidemiology, patient profile, and management
IF 3.4
4区 医学
Q2 PERIPHERAL VASCULAR DISEASE
引用次数: 0
Abstract
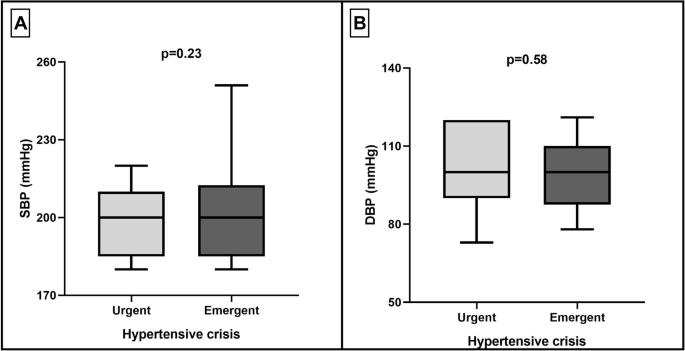
Hypertensive urgencies (HU) and hypertensive emergencies (HE) are common conditions in the cardiology emergency department (ED), often requiring urgent intervention. Despite their clinical significance, data on patient characteristics, etiologies, and management strategies remain limited. This study aimed to assess the epidemiology, clinical profile, and management of HU and HE in a tertiary cardiology ED. A single-center, observational study was conducted over 12 months, enrolling patients diagnosed with HU/HE (BP ≥ 180/120 mmHg). Demographic data, medical history, symptoms, etiologic factors, and antihypertensive treatments were recorded. Serial blood pressure (BP) measurements were taken to assess BP reduction during the ED stay. Of 4010 cardiology ED visits, 83 patients (2.1%) had HU/HE (median age 65 years, 45.8% male). Most had a history of hypertension (73.5%), with frequent coexisting smoking (56.6%) and dyslipidemia (43.4%). Common symptoms included dyspnea (19.3%) and chest pain (25.3%). Stress (26.8%) and increased salt intake (15.9%) were common etiologic factors. HE was diagnosed in 18 cases (21.7%), and 12.7% of HU cases required hospitalization. Mean BP on admission was 200/100 mmHg, with SBP and DBP reductions of 41 mmHg (−21%) and 18 mmHg (−17%), respectively. Nitrates, anxiolytics, and combination therapies resulted in the greatest BP reductions. In conclusion, HU and HE are frequently observed in hypertensive patients with additional cardiovascular risk factors. Target-organ damage is not solely related to BP levels, emphasizing the need for individualized management strategies.
心脏病急诊科的高血压急症和急诊:流行病学、患者概况和管理。
高血压急症(HU)和高血压急症(HE)是心脏病急诊科(ED)的常见病,通常需要紧急干预。尽管它们具有临床意义,但关于患者特征、病因和管理策略的数据仍然有限。本研究旨在评估三级心脏病学ED中HU和HE的流行病学、临床概况和管理。一项为期12个月的单中心观察性研究,纳入诊断为HU/HE(血压≥180/120 mmHg)的患者。记录了人口统计资料、病史、症状、病因和抗高血压治疗情况。连续测量血压(BP)以评估急诊科住院期间的血压降低情况。在4010例心脏病急诊科就诊中,83例(2.1%)患有HU/HE(中位年龄65岁,45.8%为男性)。大多数患者有高血压病史(73.5%),同时经常吸烟(56.6%)和血脂异常(43.4%)。常见症状包括呼吸困难(19.3%)和胸痛(25.3%)。压力(26.8%)和盐摄入量增加(15.9%)是常见的病因。18例(21.7%)被诊断为HE, 12.7%的HU需要住院治疗。入院时平均血压为200/100 mmHg,收缩压和舒张压分别降低41 mmHg(-21%)和18 mmHg(-17%)。硝酸盐、抗焦虑药和联合治疗的降压效果最大。综上所述,HU和HE在伴有心血管危险因素的高血压患者中较为常见。靶器官损伤并不仅仅与血压水平有关,这强调了个体化治疗策略的必要性。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Human Hypertension
医学-外周血管病
CiteScore
5.20
自引率
3.70%
发文量
126
审稿时长
6-12 weeks
期刊介绍:
Journal of Human Hypertension is published monthly and is of interest to health care professionals who deal with hypertension (specialists, internists, primary care physicians) and public health workers. We believe that our patients benefit from robust scientific data that are based on well conducted clinical trials. We also believe that basic sciences are the foundations on which we build our knowledge of clinical conditions and their management. Towards this end, although we are primarily a clinical based journal, we also welcome suitable basic sciences studies that promote our understanding of human hypertension.
The journal aims to perform the dual role of increasing knowledge in the field of high blood pressure as well as improving the standard of care of patients. The editors will consider for publication all suitable papers dealing directly or indirectly with clinical aspects of hypertension, including but not limited to epidemiology, pathophysiology, therapeutics and basic sciences involving human subjects or tissues. We also consider papers from all specialties such as ophthalmology, cardiology, nephrology, obstetrics and stroke medicine that deal with the various aspects of hypertension and its complications.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


