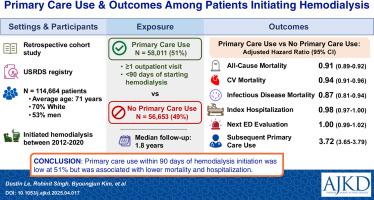
Primary Care Use and Clinical Outcomes Among Patients Initiating Hemodialysis
IF 8.2
1区 医学
Q1 UROLOGY & NEPHROLOGY
引用次数: 0
Abstract
Rationale & Objective
The association between primary care use within 90 days after hemodialysis (HD) initiation and health outcomes is unclear, so evaluating these associations may have implications for population health management. This study examined the association of primary care use after in-center HD initiation and clinical outcomes.
Study Design
Retrospective cohort study.
Setting & Participants
United States Renal Data System registry of incident patients with end-stage kidney disease linked with Medicare claims data between January 2012 and December 2020.
Exposure
Primary care use was defined as ≥1 outpatient visit to a provider with the specialty of family, general, geriatric, or internal medicine within 90 days of HD initiation.
Outcome
The primary study outcome was all-cause mortality, and secondary outcomes were cardiovascular mortality, infectious disease mortality, index hospitalization, emergency department/urgent care, kidney transplantation, intensive care unit care, and a subsequent primary care visit.
Analytical Approach
Inverse probability of treatment weighting to balance patients with primary care use with those without primary care use before fitting an unadjusted Cox proportional hazards regression model and cause-specific hazards models when competing risks were treated as censoring events.
Results
We identified 58,011 (51%) and 56,653 (49%) Medicare beneficiaries (average age 71, 70% White, and 53% men) with and without primary care use within 90 days after HD initiation, respectively. There were 58,982 deaths during a median (interquartile interval) follow-up of 1.79 (0.69-3.38) years. The hazard ratio for all-cause mortality was 0.91 (95% CI, 0.89-0.92), and there were similar reductions in cardiovascular death (HR, 0.94 [95% CI, 0.91-0.96]), infectious disease death (HR, 0.87 [95% CI, 0.81-0.94]), and index hospitalization (HR, 0.98 [95% CI, 0.97-1.00], P = 0.03). There was no difference in the next emergency department/urgent care visit (HR, 1.00 [95% CI, 0.99-1.02]), but there was an increase in receiving subsequent primary care (HR, 3.72 [95% CI, 3.65-3.79]).
Limitations
Patients had pre-existing Medicare coverage before dialysis initiation, limiting generalizability.
Conclusions
Primary care use within 90 days of HD initiation was low at 51% but was associated with lower mortality and hospitalization. Further studies are needed to assess the mechanisms and barriers of primary care use in this vulnerable population.
Plain-Language Summary
Primary care is associated with improved health outcomes for the general population, but whether this also applies to patients on dialysis is unclear. We used the United States Renal Data System database which tracks all US dialysis patients to compare those who saw a primary care provider within 3 months of starting dialysis with those who did not. We found that about 50% of patients saw a primary care provider after starting dialysis, and those who saw a primary care provider had lower rates of mortality and hospitalization. Future studies should examine how primary care use can improve outcomes and identify barriers limiting primary care use.
开始血液透析的患者的初级保健使用和临床结果
血液透析(HD)开始后90天内初级保健使用与健康结果之间的关系尚不清楚,因此评估这些关系可能对人群健康管理有影响。本研究考察了中心血液透析开始后初级保健使用与临床结果的关系。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
American Journal of Kidney Diseases
医学-泌尿学与肾脏学
CiteScore
20.40
自引率
2.30%
发文量
732
审稿时长
3-8 weeks
期刊介绍:
The American Journal of Kidney Diseases (AJKD), the National Kidney Foundation's official journal, is globally recognized for its leadership in clinical nephrology content. Monthly, AJKD publishes original investigations on kidney diseases, hypertension, dialysis therapies, and kidney transplantation. Rigorous peer-review, statistical scrutiny, and a structured format characterize the publication process. Each issue includes case reports unveiling new diseases and potential therapeutic strategies.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


