Chronic loneliness and isolation phenotypes, incident functional impairment and mortality in England between 2004 and 2018
IF 8.7
引用次数: 0
Abstract
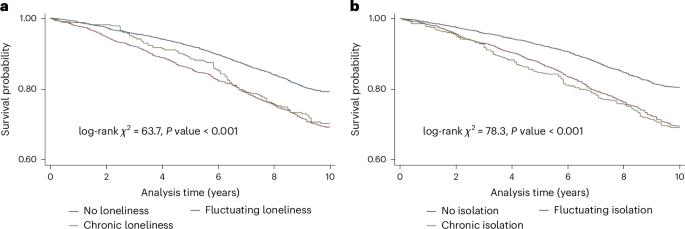
Social deficits are potential risk factors for premature mortality. Most research has focused on social deficits measured at single points in time. It remains unclear if the chronicity of loneliness affects its impact on adverse health outcomes. This study assessed the effects of chronic loneliness and isolation in predicting incident functional impairment and all-cause and cause-specific mortality. This longitudinal study used panel data from the English Longitudinal Study of Ageing, including 14 years of follow-up (waves 2–9, in 2004–2018). Social deficits over three waves (4 years) were measured using the UCLA loneliness scale and social isolation index, categorized as not present, fluctuating or chronic. We estimated the all-cause mortality risk with Cox proportional hazard modeling, and the Fine–Gray competing risk modeling was used to test the risk of functional impairment onset and cause-specific mortality. We analyzed 5,131 participants (mean age 67.6 years (s.d. 9.8)) in the mortality cohort (follow-up 9.8 years (IQR: 6.67–10.08)) and 4,279 participants (mean age 67.0 years (s.d. 9.6)) who were functional disability-free at baseline (follow-up 9.8 years (IQR: 7.17–10.17)). Compared with not being lonely/isolated, there was a higher risk of incident functional impairment among those with fluctuating loneliness (sub-hazard ratio (sHR) 1.30, 95% CI: 1.03–1.63) and chronic loneliness (sHR 1.58, 1.12–2.23), as well as chronic social isolation (sHR 1.41, 1.02–1.94). In survival analyses, compared with people who were not lonely/isolated, people experiencing fluctuating loneliness and social isolation had higher risks of all-cause mortality (loneliness HR 1.29, 1.13–1.48; isolation HR 1.15, 1.01–1.31). People with chronic isolation also had higher risks of all-cause mortality (HR 1.27, 1.05–1.55) and cancer-related mortality (sHR 1.69, 1.23–2.31). Over a 14 year follow-up, we found that chronic loneliness and isolation phenotypes were associated with aggravated risks of incident functional impairment and mortality. There was a potential dose–response relationship between chronicity of loneliness phenotypes and functional impairment onset and mortality. Preventing the onset of and transition to chronic loneliness and isolation in older age is a crucial target to support both the healthspan and the lifespan. Chronic loneliness and isolation significantly increase risks of functional impairment and mortality, as shown through longitudinal analysis of 5,131 participants using Cox proportional hazards and Fine–Gray models, highlighting the importance of addressing these social deficits in older adults.
2004年至2018年间英国的慢性孤独和隔离表型、偶发性功能障碍和死亡率。
社会缺陷是过早死亡的潜在危险因素。大多数研究都集中在单个时间点测量的社会缺陷上。目前尚不清楚孤独感的长期性是否会影响其对不良健康结果的影响。本研究评估了慢性孤独和隔离在预测意外功能损害以及全因和特定原因死亡率方面的作用。这项纵向研究使用了英国老龄化纵向研究的面板数据,包括14年的随访(2004-2018年的第2-9波)。使用加州大学洛杉矶分校孤独量表和社会隔离指数测量了三波(4年)的社会缺陷,分为不存在、波动或慢性。我们使用Cox比例风险模型估计全因死亡率风险,并使用Fine-Gray竞争风险模型来测试功能损伤发生的风险和病因特异性死亡率。我们分析了死亡率队列中的5131名参与者(平均年龄67.6岁(sd . 9.8))(随访9.8年(IQR: 6.67-10.08))和4279名基线时无功能残疾的参与者(平均年龄67.0岁(sd . 9.6))(随访9.8年(IQR: 7.17-10.17))。与不孤独/孤立的人相比,波动孤独(亚危险比(sHR) 1.30, 95% CI: 1.03-1.63)、慢性孤独(sHR 1.58, 1.12-2.23)以及慢性社会孤立(sHR 1.41, 1.02-1.94)的人发生偶发性功能障碍的风险更高。在生存分析中,与不孤独/孤立的人相比,经历波动孤独和社会孤立的人有更高的全因死亡率风险(孤独风险比1.29,1.13-1.48;分离HR 1.15, 1.01-1.31)。长期隔离的人也有更高的全因死亡率(危险比1.27,1.05-1.55)和癌症相关死亡率(危险比1.69,1.23-2.31)。在14年的随访中,我们发现慢性孤独和孤立表型与突发功能损伤和死亡率的风险增加有关。孤独感的慢性表型与功能损害的发生和死亡率之间存在潜在的剂量-反应关系。预防老年期慢性孤独和孤立的发生和过渡是支持健康寿命和寿命的关键目标。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


