Superior Semicircular Canal Dehiscence Repair With Hydroxyapetite Cement via a Transmastoid Approach
Abstract
Introduction
The aim of this study was to assess the efficacy of superior semicircular canal dehiscence (SSCD) repair via a transmastoid approach using hydroxyapatite bone cement capping.
Methods
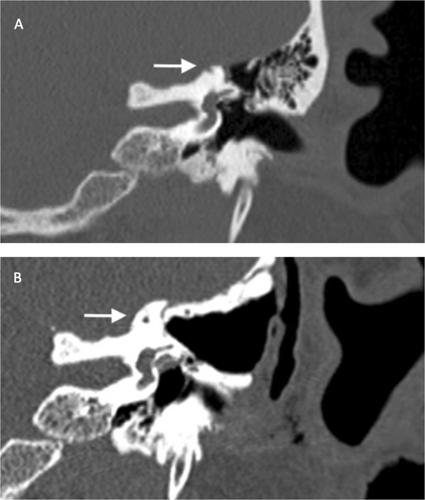
This retrospective case series was carried out at a tertiary referral center. All patients were ≥ 18-years-old diagnosed with SSCD between 2012 and 2022 and underwent a transmastoid approach implementing hydroxyapatite capping. Dehiscence location and size were assessed by reviewing preoperative CT temporal bone scans and correlated to the success rate of surgical repair. The failure rate (lack of symptom resolution and/or persistent dehiscence on postoperative imaging) and/or need for revision surgery were evaluated.
Results
Twenty-two patients (25 ears) were included. Mean age was 50.8 years (SD = 9.9 years) with 50.0% female patients (n = 11). The predominant location of SSCD was determined as apical (76.0%, n = 19), followed by anterior limb (12.0%, n = 3) and posterior limb (12.0%, n = 3). Mean dehiscence size was 2.8 mm (SD = 1.4 mm). Median follow-up time after repair was 9.0 months (interquartile range: 2–36 months). Failure rate was 8.0% (n = 2). Both cases demonstrated persistent SSCD on postoperative imaging; one case had a residual apical dehiscence of 1.6 mm persistent at 4 months, and one had a posterior-apical dehiscence of 2.3 mm persistent at 8 months after surgery.
Discussion
Transmastoid approach for SSCD repair with hydroxyapatite bone cement capping has a relatively low failure and complication rate, alleviating the need for middle fossa approach. To our knowledge, this case series represents the largest for this approach and material combination for SSCD repair, demonstrating that transmastoid repair with bone cement represents a promising approach for effective management of patients with SSCD.
Level of Evidence
4.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


