A Scoping Review of Interdisciplinary Care Programs for Women With Persistent Pelvic Pain
Abstract
Background and Objective
Persistent pelvic pain affects one in four women, with international guidelines recommending interdisciplinary care. However, much of the literature describing treatments for pelvic pain focus on the perspective of individual professions. This narrative scoping review aimed to increase understanding of interdisciplinary pelvic pain care in terms of the professions and treatment components included, coordination of care and the inclusion of people with lived experience (PWLE) in program development.
Databases and Data Treatment
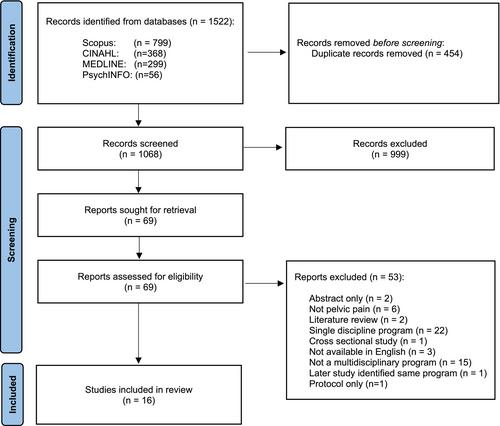
Guided by PRISMA guidelines for scoping reviews, systematic database searches were conducted in CINAHL, Scopus, Medline and PsychINFO to identify interdisciplinary programs for women with persistent pelvic pain, including pelvic pain diagnoses such as endometriosis, vulvodynia and painful bladder syndrome. Data were charted on number and type of professions (disciplines) included, treatment components, care organisation and coordination, and PWLE involvement.
Results
The search yielded 1068 records; 69 full-text articles were reviewed, and 16 studies were eligible for inclusion. Commonly included professions were physiotherapy, psychology and gynaecology. Treatment components included assessment, education and pain management strategies. Information pertaining to the coordination of care between professions and the engagement of PWLE in program development was limited.
Conclusion
This review found significant variation in the structure and components of interdisciplinary pelvic pain care programs, emphasising the need for greater consistency in their development and implementation. Further empirical research is needed to evaluate the effectiveness of specific program components. Enhanced coordination among professions and increased involvement of PWLE in program design are also recommended.
Significance Statement
This scoping review found wide variability in the processes of interdisciplinary pelvic pain care for women. Professions most frequently included were pelvic physiotherapy, psychology and gynaecology, and components most consistently included were assessment, education and pain management strategies. Coordination of care was poorly described, and people with lived experience (PWLE) were rarely involved in program development. Findings highlight the need for greater inclusion of PWLE in program design, and greater standardisation of interdisciplinary care so that outcomes can be evaluated.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


