The benefits of a department-wide prehabilitation program: A propensity score match analysis
IF 3.2
2区 医学
Q1 SURGERY
引用次数: 0
Abstract
Background
Despite increasing use of prehabilitation in aging surgical patients, large studies demonstrating benefits on postoperative outcomes are lacking. This study aimed to determine if a department-wide prehabilitation program (Surgical Prehabilitation and Readiness) improves 30-day mortality, discharge to post-acute care facilities, and postoperative length of stay in high-risk surgical patients compared to historical controls, and to examine age's influence on these outcomes.
Methods
Surgical Prehabilitation and Readiness patients with 30 days of postoperative follow-up were compared to patients from the National Surgical Quality Improvement Program database undergoing procedures at the same institution during the 5 years before Surgical Prehabilitation and Readiness implementation (pre–Surgical Prehabilitation and Readiness). Surgical Prehabilitation and Readiness patients were propensity score matched to pre–Surgical Prehabilitation and Readiness patients in a 1:3 ratio, and outcomes were compared.
Results
Over 40 months, 424 patients completed Surgical Prehabilitation and Readiness and underwent surgery with 30 days of follow-up. Compared with pre–Surgical Prehabilitation and Readiness patients, Surgical Prehabilitation and Readiness patients were significantly older (median: 69.9 vs 60.7 years, P < .001) with higher American Society of Anesthesiologists class (≥3: 84.7% vs 54.4%, P < .001) and more comorbidities. Compared to propensity score–matched pre–Surgical Prehabilitation and Readiness patients (n = 1,161), Surgical Prehabilitation and Readiness patients (n = 387) had significantly decreased 30-day mortality (0.8% vs 2.8%, P = .023), discharge to post-acute care facility (8.8% vs 12.9%, P = .030), and length of stay (7.2 vs 8.0 days, P = .039). Older Surgical Prehabilitation and Readiness patients (age > median) exhibited significantly decreased 30-day mortality (0.6% vs 3.3%, P = .044) and discharge to post-acute care facility (11.6% vs 19.3%, P = .017), whereas younger Surgical Prehabilitation and Readiness patients (age ≤ median) exhibited decreased length of stay (6.9 vs 8.2 days, P = .021).
Conclusions
Prehabilitation reduces postoperative mortality, loss of functional independence, and hospital recovery time, and the benefits vary by age. These findings support the implementation of prehabilitation programs in clinical practice.
全部门康复计划的好处:倾向评分匹配分析
背景:尽管老年外科患者越来越多地使用康复治疗,但缺乏证明其对术后结果有益的大型研究。本研究旨在确定与历史对照相比,全科范围的术前康复计划(外科术前康复和准备)是否能改善高危手术患者的30天死亡率、急症后护理设施的出院率和术后住院时间,并研究年龄对这些结果的影响。方法将术后30天随访的手术预康复和准备患者与国家外科质量改进计划数据库中实施手术预康复和准备前5年内在同一机构接受手术的患者进行比较(术前预康复和准备)。手术前康复和准备患者倾向评分与术前康复和准备患者按1:3的比例匹配,并比较结果。结果在40个月的时间里,424例患者完成了手术康复和准备,并在30天的随访中接受了手术。与术前预康复和准备就绪患者相比,术前预康复和准备就绪患者明显更老(中位数:69.9 vs 60.7岁,P <;.001),美国麻醉医师学会分级较高(≥3级:84.7% vs 54.4%, P <;.001)和更多的合并症。与倾向评分匹配的术前预适应和准备患者(n = 1,161)相比,手术预适应和准备患者(n = 387)的30天死亡率(0.8% vs 2.8%, P = 0.023),出院后急性护理设施(8.8% vs 12.9%, P = 0.030)和住院时间(7.2 vs 8.0天,P = 0.039)显著降低。老年外科康复和准备患者(年龄>;中位数)显示出30天死亡率(0.6% vs 3.3%, P = 0.044)和急性后护理设施出院(11.6% vs 19.3%, P = 0.017)显著降低,而年轻的外科康复和准备患者(年龄≤中位数)显示出住院时间缩短(6.9 vs 8.2天,P = 0.021)。结论康复治疗降低了术后死亡率、功能独立性丧失和住院康复时间,且效果因年龄而异。这些发现支持在临床实践中实施康复计划。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
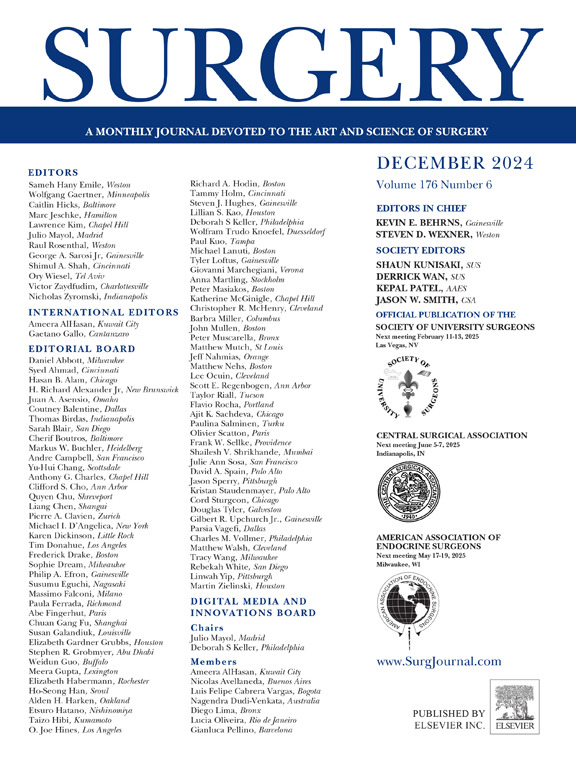
Surgery
医学-外科
CiteScore
5.40
自引率
5.30%
发文量
687
审稿时长
64 days
期刊介绍:
For 66 years, Surgery has published practical, authoritative information about procedures, clinical advances, and major trends shaping general surgery. Each issue features original scientific contributions and clinical reports. Peer-reviewed articles cover topics in oncology, trauma, gastrointestinal, vascular, and transplantation surgery. The journal also publishes papers from the meetings of its sponsoring societies, the Society of University Surgeons, the Central Surgical Association, and the American Association of Endocrine Surgeons.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


