Pulmonary vein isolation and low-voltage area ablation in sinus rhythm for persistent atrial fibrillation: The SCAR-AF randomized trial
IF 5.7
2区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
Targeting low-voltage areas (LVAs) in addition to pulmonary vein isolation (PVI) can improve ablation outcome in persistent atrial fibrillation (AF).
Objective
SCAR-AF was a multicenter, prospective, randomized trial, evaluating LVA ablation plus PVI for persistent AF.
Methods
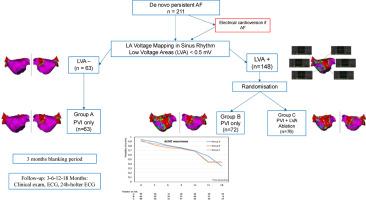
Patients with de novo persistent AF were recruited (9 referral centers in France) into the SCAR-AF study (September 2019 to August 2021). Patients without LVA were treated with PVI alone (PVI–), and those with LVA were randomized to either PVI alone (PVI+) or PVI plus LVA ablation (PVI + LVA). The primary outcome was freedom from atrial arrhythmias (AF/atrial tachycardia) after a single procedure.
Results
A total of 211 patients (73.5% men, mean ± standard deviation age 63.8 ± 9.3 years, CHA2DS2-VASc score 2.1, long-standing AF 44.5%) were included. At 18-month follow-up, the incidence of atrial-arrhythmia-free survival did not differ between groups (79.0% in PVI–, 75.7% in PVI+, and 73.1% in PVI + LVA; PVI– vs PVI+, hazard ratio (HR) 1.28, 95% confidence interval [CI] 0.64–2.55, P = .48; PVI+ vs PVI + LVA, HR 1.28; 95% CI 0.67–2.45, P = .45). On multivariable analysis, presence of LVA was associated with advancing age (HR 1.11, 95% CI 1.06–1.16, P < .001) and was inversely correlated with body mass index (HR 0.93, 95% CI 0.87–0.99, P = .029) and smoking.
Conclusion
In this randomized trial, PVI plus LVA ablation did not improve outcomes in patients with persistent AF. LVA may represent a marker of atrial cardiomyopathy, but its presence does not seem to be an effective target in persistent AF.
肺静脉隔离和低压区消融在窦性心律治疗持续性心房颤动:SCAR-AF随机试验。
背景:针对低压区(LVA)和肺静脉隔离(PVI)可以改善持续性心房颤动(AF)的消融结果。目的:SCAR-AF是一项多中心、前瞻性、随机试验,评估LVA消融加PVI治疗持续性房颤的效果。方法:招募复发性持续性房颤患者(法国9个转诊中心)参与SCAR-AF研究(2019年9月至2021年8月)。无LVA的患者单独接受PVI治疗(PVI-),有LVA的患者随机分为单独接受PVI治疗(PVI+)或PVI+LVA消融治疗(PVI+LVA)。主要结局是单次手术后无房性心律失常(AF/房性心动过速)。结果:共纳入211例患者,其中男性73.5%,平均±SD年龄63.8±9.3岁,CHA2DS2-VASc评分2.1,长期AF 44.5%。在18个月的随访中,两组间无房性心律失常生存率无差异(PVI- 79.0%, PVI+ 75.7%, PVI+LVA 73.1%;PVI- vs PVI+:风险比(HR) 1.28;95%置信区间[CI] 0.64-2.55, P= 0.48;PVI+ vs PVI+LVA: HR 1.28;95% ci 0.67-2.45;P =。45)。在多变量分析中,LVA的存在与年龄增长相关(HR 1.11, CI 1.06-1.16;结论:在这项随机试验中,PVI + LVA消融并没有改善持续性房颤患者的预后。LVA可能是心房心肌病的一个标志,但它的存在似乎不是持续性房颤的有效靶点。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Heart rhythm
医学-心血管系统
CiteScore
10.50
自引率
5.50%
发文量
1465
审稿时长
24 days
期刊介绍:
HeartRhythm, the official Journal of the Heart Rhythm Society and the Cardiac Electrophysiology Society, is a unique journal for fundamental discovery and clinical applicability.
HeartRhythm integrates the entire cardiac electrophysiology (EP) community from basic and clinical academic researchers, private practitioners, engineers, allied professionals, industry, and trainees, all of whom are vital and interdependent members of our EP community.
The Heart Rhythm Society is the international leader in science, education, and advocacy for cardiac arrhythmia professionals and patients, and the primary information resource on heart rhythm disorders. Its mission is to improve the care of patients by promoting research, education, and optimal health care policies and standards.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


