Efficacy and Safety of Bronchoscopic Lung Volume Reduction With Endobronchial Valves: A Systematic Review and Meta-analysis
Q4 Medicine
引用次数: 0
Abstract
Introduction
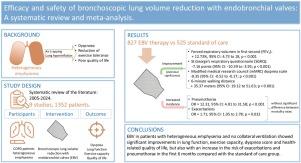
Emphysema is a phenotype of chronic obstructive pulmonary disease (COPD) that causes air trapping and lung hyperinflation and, consequently, dyspnea, reduced exercise tolerance, and poor health-related quality of life. Several randomized controlled clinical trials have shown that bronchoscopic lung volume reduction (BLVR) with endobronchial valves (EBV) achieves clinically relevant improvements in dyspnea, pulmonary function, exercise capacity and quality of life 12 months after valve implantation in patients with heterogeneous emphysema without collateral ventilation. The goal of our meta-analysis is to examine the efficacy and safety of BLRV in patients with COPD.
Material and methods
A literature search was performed with PubMed, Embase and Cochrane to identify randomized controlled trials on BLVR with endobronchial valves published from 2005 onwards.
Results
Nine studies with a total of 1352 patients were included; 827 received EBV therapy and 525 standard of care (SOC) medications. The first group showed statistically significant improvements in forced expiratory volume in 1 second (FEV1), Saint George Respiratory Questionnaire (SGRQ) score, modified medical research council (mMRC) dyspnea scale, and 6-minute walk distance (6MWD), and a statistically significant reduction in residual volume (RV). The incidence of pneumothorax and exacerbations in the EBV arm increase significantly, and there were no significant difference between mortality rates.
Conclusions
Patients with heterogeneous emphysema and no collateral ventilation showed significant improvements in lung function, exercise capacity, dyspnea score, and health-related quality of life after BLVR-EBV, although the risk of exacerbations and pneumothorax in the first 6 months increased compared with the group receiving standard care.
支气管镜下支气管内瓣膜肺减容术的疗效和安全性:一项系统综述和荟萃分析
肺气肿是慢性阻塞性肺疾病(COPD)的一种表型,可导致空气困住和肺部恶性膨胀,从而导致呼吸困难、运动耐量降低和健康相关生活质量差。几项随机对照临床试验表明,支气管镜下肺减容(BLVR)联合支气管内瓣膜(EBV)在非侧支通气的异质性肺气肿患者植入瓣膜后12个月,在呼吸困难、肺功能、运动能力和生活质量方面取得了临床相关的改善。我们荟萃分析的目的是检查BLRV在COPD患者中的疗效和安全性。材料与方法通过PubMed、Embase和Cochrane检索2005年以来发表的支气管内瓣膜BLVR的随机对照试验。结果纳入9项研究,共1352例患者;827例接受EBV治疗,525例接受标准护理(SOC)药物治疗。第一组患者1秒用力呼气量(FEV1)、圣乔治呼吸问卷(SGRQ)评分、改良医学研究委员会(mMRC)呼吸困难量表、6分钟步行距离(6MWD)改善有统计学意义,残气量(RV)降低有统计学意义。EBV组气胸和病情加重的发生率显著增加,死亡率之间无显著差异。结论非侧支通气的异质性肺气肿患者在BLVR-EBV治疗后肺功能、运动能力、呼吸困难评分和健康相关生活质量均有显著改善,但与接受标准治疗的患者相比,前6个月病情恶化和气胸的风险增加。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Open Respiratory Archives
Medicine-Pulmonary and Respiratory Medicine
CiteScore
1.10
自引率
0.00%
发文量
58
审稿时长
51 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


