Simplified computed tomography pulmonary angiography score predicts clinical deterioration in patients with acute pulmonary embolism
IF 2.5
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
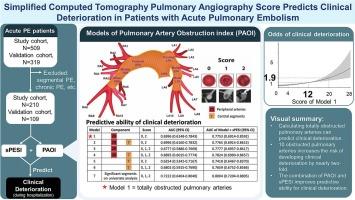
Currently, simplified methods based on computed tomography pulmonary angiography (CTPA) to predict clinical deterioration in patients with acute pulmonary embolism (PE) are lacking. We developed a simplified imaging model with good clinical accessibility to predict this outcome.
Study design and methods
Patients with acute pulmonary embolism from 2008 to 2019 were retrospectively enrolled from two medical centers to form a study cohort and a validation cohort. Seven models of pulmonary artery obstruction index (PAOI) were developed based on the location and degree of obstruction. The outcome of interest was clinical deterioration during hospitalization. Logistic regression analysis was used to assess the association between different models and clinical deterioration. The category-free net reclassification improvement (NRI) and integrated discrimination improvement (IDI) were used to quantify improvements in predictability.
Results
The study group included 210 patients (mean age: 65 ± 16 years; male: 40 %) and the external validation group included 109 patients (mean age: 64 ± 17 years; male: 43 %). Calculating the nearly total obstruction of 20 peripheral arteries demonstrated good predictive ability (AUC: 0.77). Total obstruction of six peripheral arteries did not increase the odds of clinical deterioration, while total obstruction of ten peripheral arteries nearly doubled the risk of deterioration. Combining PAOI with the simplified pulmonary embolism severity index (sPESI) improved the predictive ability for clinical deterioration compared to using sPESI alone (NRI: 0.09–0.12; IDI: 0.05–0.09).
Conclusion
Calculating totally obstructed pulmonary arteries simplifies the prediction of clinical deterioration. The combination of PAOI and sPESI enhances the ability to predict clinical deterioration in patients with acute PE.
简化计算机断层肺血管造影评分预测急性肺栓塞患者的临床恶化
目前,基于计算机断层肺血管造影(CTPA)的预测急性肺栓塞(PE)患者临床恶化的简化方法尚缺乏。我们开发了一种简化的成像模型,具有良好的临床可及性来预测这种结果。研究设计和方法回顾性纳入2008年至2019年两个医疗中心的急性肺栓塞患者,形成研究队列和验证队列。根据肺动脉阻塞的位置和程度,建立了7种肺动脉阻塞指数(PAOI)模型。关注的结果是住院期间的临床恶化。采用Logistic回归分析评估不同模型与临床恶化的关系。使用无类别净重分类改进(NRI)和综合区分改进(IDI)来量化可预测性的改进。结果研究组纳入210例患者,平均年龄65±16岁;男性:40%),外部验证组包括109例患者(平均年龄:64±17岁;男性:43%)。计算20条外周动脉的几乎全部梗阻具有良好的预测能力(AUC: 0.77)。6条外周动脉的完全阻塞没有增加临床恶化的几率,而10条外周动脉的完全阻塞几乎使恶化的风险增加了一倍。与单独使用sPESI相比,PAOI联合简化肺栓塞严重程度指数(sPESI)提高了临床恶化的预测能力(NRI: 0.09-0.12;伊迪:0.05 - -0.09)。结论计算肺动脉完全阻塞可简化病情恶化的预测。PAOI和sPESI的结合提高了对急性PE患者临床恶化的预测能力。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

IJC Heart and Vasculature
Medicine-Cardiology and Cardiovascular Medicine
CiteScore
4.90
自引率
10.30%
发文量
216
审稿时长
56 days
期刊介绍:
IJC Heart & Vasculature is an online-only, open-access journal dedicated to publishing original articles and reviews (also Editorials and Letters to the Editor) which report on structural and functional cardiovascular pathology, with an emphasis on imaging and disease pathophysiology. Articles must be authentic, educational, clinically relevant, and original in their content and scientific approach. IJC Heart & Vasculature requires the highest standards of scientific integrity in order to promote reliable, reproducible and verifiable research findings. All authors are advised to consult the Principles of Ethical Publishing in the International Journal of Cardiology before submitting a manuscript. Submission of a manuscript to this journal gives the publisher the right to publish that paper if it is accepted. Manuscripts may be edited to improve clarity and expression.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


