The clinical and electrocardiographic phenotype of patients with genotype-negative long QT syndrome
IF 5.7
2区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
Long QT syndrome (LQTS) is a genetic heart disease that increases the risk of ventricular arrhythmias and sudden cardia arrest. Despite advances in genetic testing, a small subset of patients with LQTS remain genetically elusive.
Objective
This study aimed to determine the prevalence and clinical characteristics of patients with a phenotype of LQTS but without a genotype.
Methods
This study aimed to identify phenotype-positive, genotype-negative patients with LQTS seen at Mayo Clinic (2000–2024). Retrospective data included demographics, clinical evaluations, electrocardiograms, and genetic results. Diagnosis adhered to established criteria, and genotype-negative LQTS was defined by the absence of pathogenic variants despite clinical presentation.
Results
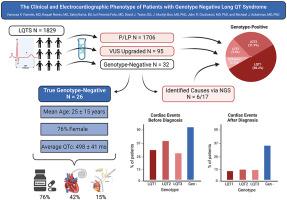
The study included 1829 patients with LQTS. Of these, 1706 (93%) had pathogenic or likely pathogenic variants, and 95 patients (5%) had upgraded clinical variants of uncertain significance, leaving 32 (1.7%) with negative genetic tests. Among the genotype-negative patients, 17 underwent next-generation sequencing, identifying a genetic cause in 6 cases (0.3% of the total). The mean age at diagnosis for the remaining 26 patients was 25 ± 15 years, with 76% being women and an average initial corrected QT of 498 ± 41 ms. Fourteen patients (53%) experienced cardiac events prior to diagnosis, and 11 (44%) received an implantable cardioverter-defibrillator. The mean follow-up period was 8 ± 7 years.
Conclusion
Genotype-negative LQTS accounted for < 2% of our cohort, highlighting diagnostic and management challenges. Comprehensive clinical evaluation and advanced genetic testing remain essential for accurate diagnosis and care.
基因型阴性长QT综合征患者的临床和心电图表型。
背景:长QT综合征(LQTS)是一种遗传性心脏病,可增加室性心律失常和心搏骤停的风险。尽管基因检测取得了进步,但一小部分LQTS患者的基因仍然难以捉摸。目的:了解LQTS表型但基因型阴性患者的患病率及临床特点。方法:本研究旨在鉴定2000 - 2024年在梅奥诊所(Mayo Clinic)就诊的表型阳性、基因型阴性的LQTS患者。回顾性数据包括人口统计学、临床评估、心电图和遗传结果。诊断遵循既定标准,基因型阴性LQTS的定义是,尽管临床表现,但没有致病变异。结果:本研究纳入1829例LQTS患者。其中,1706例(93%)有致病性或可能致病性变异,95例(5%)有不确定意义的升级临床变异,剩下32例(1.7%)基因检测呈阴性。在基因型阴性患者中,17例接受了新一代测序,其中6例(占总数的0.3%)确定了遗传原因。其余26例患者的平均诊断年龄为25±15岁,76%为女性,平均初始QTc为498±41 ms。14名患者(53%)在诊断前经历过心脏事件,11名患者(44%)接受了植入式心律转复除颤器(ICD)。平均随访时间为8±7年。结论:LQTS占基因型阴性
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Heart rhythm
医学-心血管系统
CiteScore
10.50
自引率
5.50%
发文量
1465
审稿时长
24 days
期刊介绍:
HeartRhythm, the official Journal of the Heart Rhythm Society and the Cardiac Electrophysiology Society, is a unique journal for fundamental discovery and clinical applicability.
HeartRhythm integrates the entire cardiac electrophysiology (EP) community from basic and clinical academic researchers, private practitioners, engineers, allied professionals, industry, and trainees, all of whom are vital and interdependent members of our EP community.
The Heart Rhythm Society is the international leader in science, education, and advocacy for cardiac arrhythmia professionals and patients, and the primary information resource on heart rhythm disorders. Its mission is to improve the care of patients by promoting research, education, and optimal health care policies and standards.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


