Alcoholic Hepatitis in a Japanese Hospital: Losing Contact With Some Patients After Delirium Tremens May Lead to Missed Critical Events
Abstract
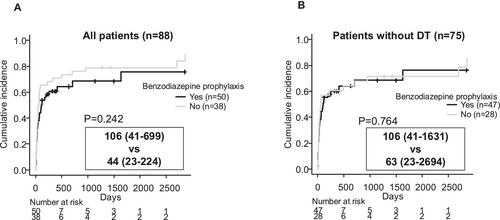
In Japan, the establishment of diagnostic criteria for acute-on-chronic liver failure (ACLF) in 2022 has increased the focus on alcoholic hepatitis. Most hospitals in Japan lack specialized treatment units or psychiatrists for managing alcohol use disorders, leaving hepatologists to handle various aspects of the disease—a challenging task. This study retrospectively investigated the outcomes of alcoholic hepatitis in a typical Japanese hospital setting, stratified by ACLF diagnosis and other features, with the aim of identifying areas for possible improvement. We conducted a retrospective analysis of 88 patients hospitalized with alcoholic hepatitis, reviewing records for the diagnosis of ACLF or related conditions, development of delirium tremens (DT), risk factors, and patient outcomes. Patients meeting the Japanese criteria for ACLF or related conditions had significantly worse survival outcomes. DT developed in 13 patients, with low platelet counts and elevated γ-glutamyl transpeptidase levels identified as risk factors. Prophylactic oral benzodiazepines were found safe and significantly associated with preventing DT. Onset of DT during hospitalization did not measurably impact survival prognosis, but DT patients showed a tendency to break contact with our hospital and critical events may have been missed. While under hepatologist care, patients typically maintained sobriety, but relapse into alcohol-related health problems frequently occurred after follow-up was discontinued. In Japan, hepatologists may be missing important events with alcoholic hepatitis after follow-up discontinuation, especially in patients with DT. Therefore, integrated and collaborative care, particularly a psychosocial approach providing behavioural support, may reduce risk of relapse and improve patient prognosis.
Trial Registration:
All study protocols were reviewed and approved by the ethics committee at Fujita Health University School of Medicine (approval no. HM23-213)

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


