How many cases of spinal intramedullary ependymoma surgery are required to achieve stability? - Analysis using X-bar charts
IF 2.2
4区 医学
Q3 CLINICAL NEUROLOGY
引用次数: 0
Abstract
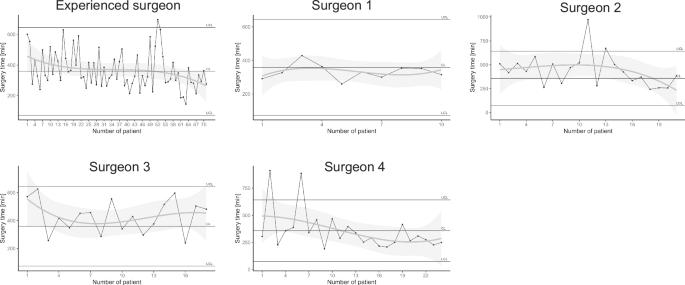
Retrospective cohort study. To evaluate surgical consistency and clinical outcomes in intramedullary ependymoma (WHO grade II) cases by using X-bar charts as a tool to assess procedural stability. The single institution in Japan. This study included patients who underwent resection of intramedullary ependymomas between 2001 and 2023. All surgeries were performed by one of five board-certified spine surgeons. Operative time was analyzed for stability using X-bar charts. Neurological outcomes were assessed using the modified McCormick Scale (mMS), and regression analysis was performed to evaluate the relationship between operative time and mMS. The study included 144 patients (82 men, 62 women; average age 50.3 ± 14.6 years). Tumors were located at cervical (67.4%) or thoracic (32.6%) levels, averaging 3.0 ± 1.2 vertebrae. The surgeon who performed 71 cases was defined as the experienced surgeon, and the other surgeons performed 10–24 cases, respectively. The mean operative time was 380.6 ± 140.7 min, and 135 cases achieved gross total resection. The average follow-up duration was 6.9 ± 3.9 years. X-bar charts showed surgical stability once the average number of cases exceeded 17. No significant correlation was found between operative time and mMS for any surgeon. Perioperative complications were minimal. X-bar charts are a valuable tool for objectively evaluating surgical stability. In intramedullary ependymoma surgeries, consistency in operative time was achieved after 17 cases, and longer procedures did not adversely affect neurological outcomes. This method could be extended to monitor procedural reliability in other complex surgical interventions.
多少例脊髓髓内室管膜瘤需要手术才能达到稳定?-使用x柱状图进行分析。
研究设计:回顾性队列研究。目的:通过x柱图作为评估手术稳定性的工具,评估髓内室管膜瘤(WHO II级)病例的手术一致性和临床结果。背景:日本唯一的机构。方法:本研究纳入了2001年至2023年间行髓内室管膜瘤切除术的患者。所有手术均由五位经委员会认证的脊柱外科医生中的一位进行。使用x柱状图分析手术时间的稳定性。采用改良的McCormick量表(mMS)评估神经系统预后,并进行回归分析评估手术时间与mMS的关系。结果:共纳入144例患者(男性82例,女性62例;平均年龄(50.3±14.6岁)。肿瘤位于颈椎(67.4%)或胸椎(32.6%)水平,平均3.0±1.2椎体。其中71例为经验丰富的外科医生,其他外科医生分别为10-24例。平均手术时间为380.6±140.7 min, 135例实现全切。平均随访时间为6.9±3.9年。x柱状图显示平均病例数超过17例时手术稳定性。任何外科医生的手术时间与mMS均无显著相关性。围手术期并发症极少。结论:x柱状图是客观评价手术稳定性的有效工具。在髓内室管膜瘤手术中,17例手术时间一致,更长的手术时间对神经系统预后没有不利影响。该方法可扩展到其他复杂手术干预的程序可靠性监测。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Spinal cord
医学-临床神经学
CiteScore
4.50
自引率
9.10%
发文量
142
审稿时长
2 months
期刊介绍:
Spinal Cord is a specialised, international journal that has been publishing spinal cord related manuscripts since 1963. It appears monthly, online and in print, and accepts contributions on spinal cord anatomy, physiology, management of injury and disease, and the quality of life and life circumstances of people with a spinal cord injury. Spinal Cord is multi-disciplinary and publishes contributions across the entire spectrum of research ranging from basic science to applied clinical research. It focuses on high quality original research, systematic reviews and narrative reviews.
Spinal Cord''s sister journal Spinal Cord Series and Cases: Clinical Management in Spinal Cord Disorders publishes high quality case reports, small case series, pilot and retrospective studies perspectives, Pulse survey articles, Point-couterpoint articles, correspondences and book reviews. It specialises in material that addresses all aspects of life for persons with spinal cord injuries or disorders. For more information, please see the aims and scope of Spinal Cord Series and Cases.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


