Risk factors, prenatal diagnosis, and outcome of posterior placenta accreta spectrum disorders in patients with placenta previa or low-lying placenta: A multicenter study
Abstract
Introduction
Placenta accreta spectrum (PAS) disorders occur when the definitive placenta develops within the uterus scar area. Although classically PAS develops in the anterior wall of the uterus mainly, it can also develop in the posterior uterine wall. The aim of this study was to report the risk factors, diagnostic accuracy of prenatal imaging, and surgical outcome of pregnancies complicated by posterior PAS in women with placenta previa or low-lying.
Material and Methods
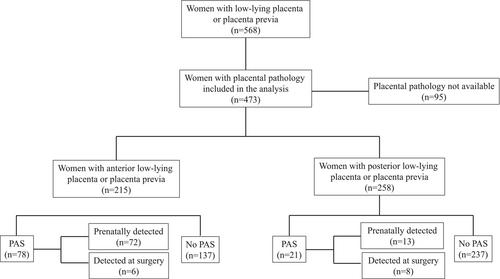
Secondary analysis of a multicenter prospective study involving 16 referral hospitals in Italy (ADoPAD Study). Inclusion criteria were patients with a posterior low-lying placenta (<20 mm from the internal cervical os) or placenta previa (covering the os), aged ≥18 years undergoing ultrasound assessment at ≥26+0 weeks of gestation. The reference standard for PAS was represented by the failure of placental separation at delivery or by pathological analysis. The primary aim was to report the risk factors associated with the occurrence of posterior PAS. The secondary aims were to evaluate the ability of prenatal ultrasound in detecting posterior PAS and to report its surgical outcome compared to posterior placental previa or low-lying with no PAS and anterior PAS, respectively, and in patients with a prenatal compared to post-natal diagnosis. Univariate and diagnostic accuracy analyses were used to analyze the data.
Results
258 patients were included in the analysis. Posterior PAS occurred in 8.1% (n = 21; 95% CI 5.4–12.1) of patients. There was a higher incidence of one or more prior CS (62% vs. 21%, p < 0.001) and myomectomy with uterine penetration (71.0% vs. 3.4%, p < 0.001) in patients with posterior PAS compared to those with no PAS. In patients with posterior PAS, placenta accreta occurred in 66.67% (14/21), increta in 23.81% (5/21), and percreta in 9.52% (2/21) of cases. Posterior PAS confirmed at birth was diagnosed prenatally by ultrasound in 62% (13/21) of cases. When comparing anterior with posterior PAS, patients with anterior PAS were more likely to have a prior CS (82% vs. 62%; p = 0.0049) and placenta percreta (54% vs. 10%; p < 0.001). Finally, the need for hysterectomy (89% vs. 48%; p < 0.001) was higher, while that of balloon tamponade insertion was lower (17% vs. 52%; p = 0.001) in patients with anterior compared to posterior PAS.
Conclusions
Prior uterine surgery in patients with placenta previa or low-lying represents the commonest risk factors for posterior PAS. The diagnostic accuracy of ultrasound in detecting posterior PAS is lower in cases with posterior compared to anterior PAS. Finally, in referral centers, posterior PAS disorders were associated with a lower risk of hysterectomy compared to anterior PAS.




 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


