Structural weight stigma in healthcare toward preconception, pregnant, and postpartum women: A systematic review
Abstract
Introduction
Structural weight stigma for reproductive-aged women can limit healthcare access and increase physical and mental health concerns, with adverse intergenerational outcomes. The aim of this systematic review was to synthesize evidence of structural weight stigma in healthcare and determine how that impacts the care for women across the preconception, pregnant, and postpartum periods.
Methodology
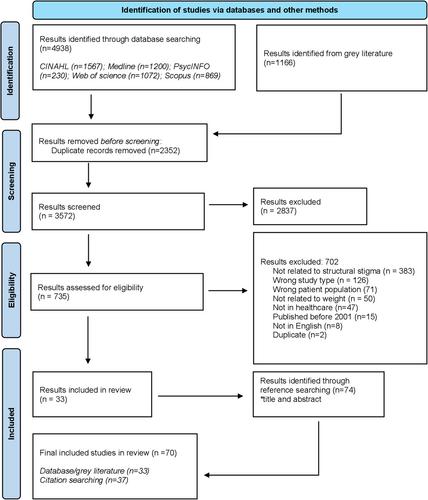
The concepts of stigma, weight, healthcare, and women of reproductive age were combined and searched in five databases (Ovid Medline, PsycINFO, Web of Science, Scopus, CINAHL) and 12 gray literature sources. Inclusion criteria consisted of any peer-reviewed study or government policy that described a structural element within healthcare (e.g., guidelines, funding, insurance, equipment, physical environment) relevant to women of reproductive age (18–50 years) between 2001 and 2023. A narrative synthesis using a convergent approach was employed to analyze results.
Results
A total of 70 studies were included in this review; 24 qualitative, 21 quantitative, 10 policies, 3 dissertations, and one mixed-method study. Structural weight stigma in healthcare presented across: 1) institutional policies that are weight-centric and often placed women in larger bodies on “high-risk” pathways; 2) the lack of government funding and insurance coverage for weight-related services; 3) uncertainty amongst healthcare professions regarding their roles and responsibilities, 4) stigmatizing physical environments; and 5) lack of appropriately sized equipment.
Conclusions
Structural weight stigma impacting preconception, pregnant and postpartum women living in larger bodies was highly prevalent. Reducing structural weight stigma is important to improve healthcare access and improve the quality of care.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


