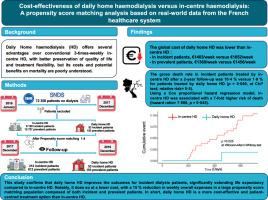
Cost-effectiveness of daily home haemodialysis versus in-centre haemodialysis: A propensity score matching analysis based on real-world data from the French healthcare system
IF 6.1
2区 医学
Q1 MEDICINE, GENERAL & INTERNAL
引用次数: 0
Abstract
Background Daily home haemodialysis (HD) offers several advantages over conventional 3-times-weekly in-centre HD, with better preservation of quality of life and treatment flexibility, but its costs and potential benefits on mortality are poorly understood.
Methods Individual healthcare data from the French National Health Data System for patients with end-stage kidney disease undergoing dialysis cross-referenced with the French National Cost Scale of the health ministry. After exclusion of patients treated < 90 days, and those without a treatment schedule or incomplete data for a social disadvantage score, 42 605 patients were selected (28 317 prevalent and 14 288 incident HD patients). After propensity score matching, 265 incident patients (in-centre HD, n = 212; daily home HD, n = 53) and 765 prevalent patients (in-centre HD, n = 612; daily home HD, n = 153) were analysed.
Findings The global cost of daily home HD in incident patients was lower than in-centre HD (€1403/week vs. €1652/week, respectively). In prevalent patients, the cost was also slightly lower for daily home haemodialysis than compared to in-centre haemodialysis (€1360/week vs. €1456/week, respectively).
The gross death rate in incident patients treated by in-centre HD after a 2-year follow-up was 10·4 % vs. 1·9 % for patients treated by daily home HD (p = 0·049, at Chi2 test; relative risk=5·5). Using a Cox proportional hazard regression model, in-centre HD was associated with a 7-fold higher risk of death (hazard ratio=7·888, p = 0·045).
Interpretation Daily home HD is a more cost-effective and patient-centred treatment option than in-centre HD.
Funding This research was funded by Physidia Ltd and Ramsay Health Care, France.
每日家庭血液透析与中心血液透析的成本效益:基于法国医疗保健系统真实数据的倾向评分匹配分析。
与传统的每周3次的中心血液透析相比,每日家庭血液透析(HD)有几个优点,可以更好地保存生活质量和治疗灵活性,但其成本和对死亡率的潜在益处尚不清楚。方法法国国家健康数据系统中透析终末期肾病患者的个人健康数据与卫生部的法国国家成本量表进行交叉对照。在排除治疗< 90天的患者,以及没有治疗计划或社会劣势评分数据不完整的患者后,选择了42 605例患者(28 317例常见HD患者和14 288例意外HD患者)。倾向评分匹配后,265例事件患者(中心HD, n = 212;每日家庭HD, n = 53)和765例流行患者(中心HD, n = 612;每日家庭HD, n = 153)进行分析。突发事件患者每日家庭HD的全球成本低于中心HD(分别为1403欧元/周和1652欧元/周)。在流行患者中,每日家庭血液透析的成本也略低于中心血液透析(分别为1360欧元/周和1456欧元/周)。在2年随访后,接受中心HD治疗的患者的总死亡率为10.4%,而每日家庭HD治疗的患者的总死亡率为1.9% (p = 0.049,在ch2检验中;相对风险= 5·5)。使用Cox比例风险回归模型,中心HD与7倍高的死亡风险相关(风险比= 7.888,p = 0.045)。口译每日家庭高清比中心高清更具成本效益和以患者为中心的治疗选择。本研究由Physidia Ltd和Ramsay Health Care, France资助。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
9.60
自引率
6.20%
发文量
364
审稿时长
20 days
期刊介绍:
The European Journal of Internal Medicine serves as the official journal of the European Federation of Internal Medicine and is the primary scientific reference for European academic and non-academic internists. It is dedicated to advancing science and practice in internal medicine across Europe. The journal publishes original articles, editorials, reviews, internal medicine flashcards, and other relevant information in the field. Both translational medicine and clinical studies are emphasized. EJIM aspires to be a leading platform for excellent clinical studies, with a focus on enhancing the quality of healthcare in European hospitals.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


