Treatment-related mutagenic processes in acute lymphoblastic leukemia.
IF 8.2
1区 医学
Q1 HEMATOLOGY
引用次数: 0
Abstract
Karyotyping, SNP arrays, fluorescence in situ hybridisation and next generation sequencing techniques have greatly improved our understanding of the genetic drivers of acute lymphoblastic leukemia (ALL). In the past years, another layer of genetic data has been added by the study of mutational signatures, patterns of somatic mutations that represent specific mutational mechanisms. Mutational signatures can give insight in tumor development, but also reveal mutagenic side-effects of treatment in relapse samples. Multiple treatment-related mutational signatures have been detected in relapsed ALL that could play a role in therapy resistance and relapse development. In fact, multiple pathogenic driver mutations have been attributed to these treatment-related mutational processes, including a recurrent TP53 mutation. Studies in childhood ALL revealed that thiopurine exposure is the most common source of therapy-related mutagenicity in ALL and presents differently when patients are DNA mismatch repair deficient. Thiopurine-induced DNA damage indicates that leukemic cells were able to survive thiopurine exposure. This could be due to metabolic defects, acquired mutations that induce thiopurine resistance during treatment or resistance to drugs synergizing with thiopurines. In this review, we discuss the types and prevalence of treatment-related mutational signatures in ALL, and explore mechanisms of thiopurine cytotoxicity and mutagenicity.急性淋巴细胞白血病治疗相关的致突变过程。
核型、SNP阵列、荧光原位杂交和下一代测序技术极大地提高了我们对急性淋巴细胞白血病(ALL)遗传驱动因素的理解。在过去的几年里,另一层遗传数据已经通过突变特征的研究增加了,体细胞突变模式代表了特定的突变机制。突变特征可以提供肿瘤发展的洞察力,但也揭示了治疗复发样本的诱变副作用。在复发性ALL中发现了多种治疗相关的突变特征,这些突变可能在治疗抵抗和复发发展中发挥作用。事实上,多种致病驱动突变归因于这些与治疗相关的突变过程,包括复发性TP53突变。对儿童ALL的研究表明,硫嘌呤暴露是ALL中最常见的治疗相关突变性来源,当患者DNA错配修复缺陷时表现不同。硫嘌呤诱导的DNA损伤表明白血病细胞能够在硫嘌呤暴露下存活。这可能是由于代谢缺陷,获得性突变在治疗期间诱导硫嘌呤耐药或对与硫嘌呤协同作用的药物耐药。在这篇综述中,我们讨论了ALL中治疗相关突变特征的类型和流行,并探讨了硫嘌呤细胞毒性和致突变性的机制。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Haematologica
医学-血液学
CiteScore
14.10
自引率
2.00%
发文量
349
审稿时长
3-6 weeks
期刊介绍:
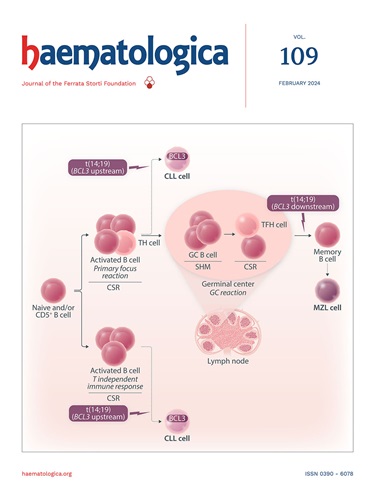
Haematologica is a journal that publishes articles within the broad field of hematology. It reports on novel findings in basic, clinical, and translational research.
Scope:
The scope of the journal includes reporting novel research results that:
Have a significant impact on understanding normal hematology or the development of hematological diseases.
Are likely to bring important changes to the diagnosis or treatment of hematological diseases.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


