Targeting the glioblastoma resection margin with locoregional nanotechnologies
IF 82.2
1区 医学
Q1 ONCOLOGY
引用次数: 0
Abstract
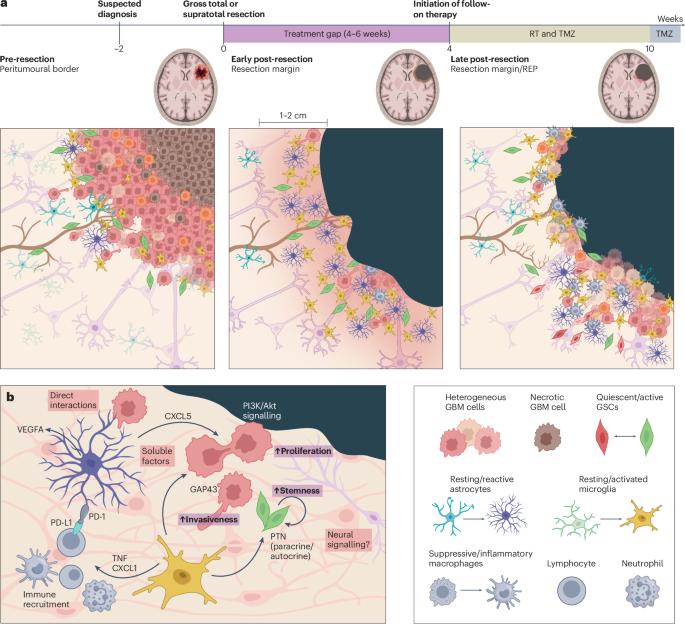
Surgical resection is the first stage of treatment for patients diagnosed with resectable glioblastoma and is followed by a combination of adjuvant radiotherapy and systemic single-agent chemotherapy, which is typically commenced 4–6 weeks after surgery. This delay creates an interval during which residual tumour cells residing in the resection margin can undergo uninhibited proliferation and further invasion, even immediately after surgery, thus limiting the effectiveness of adjuvant therapies. Recognition of the postsurgical resection margin and peri-marginal zones as important anatomical clinical targets and the need to rethink current strategies can galvanize opportunities for local, intraoperative approaches, while also generating a new landscape of innovative treatment modalities. In this Perspective, we discuss opportunities and challenges for developing locoregional therapeutic strategies to target the glioblastoma resection margin as well as emerging opportunities offered by nanotechnology in this clinically transformative setting. We also discuss how persistent barriers to clinical translation can be overcome to offer a potential path forward towards broader acceptability of such advanced technologies. Patients with resectable glioblastoma undergo upfront surgery followed by adjuvant radiotherapy plus chemotherapy. This approach implies a period of approximately 4–6 weeks between surgery and the start of adjuvant therapy in which the patient receives no active treatment. In this Perspective, the authors describe the potential of local therapies targeting the tumour resection margin that can be administered during this time window, including biological feasibility, the potential role of nanomedicines and various technical and regulatory challenges that will need to be addressed before clinical implementation becomes feasible.

局部纳米技术靶向胶质母细胞瘤切除边缘
手术切除是可切除胶质母细胞瘤患者的第一阶段治疗,随后是辅助放疗和全身单药化疗的联合治疗,通常在手术后4-6周开始。这种延迟造成了一个间隔,在此期间,残留在切除边缘的肿瘤细胞可以不受抑制地增殖和进一步侵袭,甚至在手术后立即发生,从而限制了辅助治疗的有效性。认识到术后切除边缘和边缘周围区域是重要的解剖学临床目标,需要重新思考当前的策略,可以激发局部,术中入路的机会,同时也产生了创新治疗模式的新景观。在这个观点中,我们讨论了发展局部区域治疗策略的机遇和挑战,以靶向胶质母细胞瘤切除边缘,以及纳米技术在这个临床变革环境中提供的新兴机会。我们还讨论了如何克服临床翻译的持续障碍,为这种先进技术的更广泛可接受性提供潜在的途径。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
99.40
自引率
0.40%
发文量
114
审稿时长
6-12 weeks
期刊介绍:
Nature Reviews publishes clinical content authored by internationally renowned clinical academics and researchers, catering to readers in the medical sciences at postgraduate levels and beyond. Although targeted at practicing doctors, researchers, and academics within specific specialties, the aim is to ensure accessibility for readers across various medical disciplines. The journal features in-depth Reviews offering authoritative and current information, contextualizing topics within the history and development of a field. Perspectives, News & Views articles, and the Research Highlights section provide topical discussions, opinions, and filtered primary research from diverse medical journals.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


