Genetic variants and characterization of MODY in a single, large pediatric referral center
IF 3.3
Q1 ENDOCRINOLOGY & METABOLISM
Journal of Clinical and Translational Endocrinology
Pub Date : 2025-05-10
DOI:10.1016/j.jcte.2025.100398
引用次数: 0
Abstract
Background
Identifying Maturity-onset diabetes of the young (MODY) is essential as treatment differs from other forms of diabetes. Clinical characteristics and MODY probability calculator (MPC) scores were evaluated in patients with MODY.
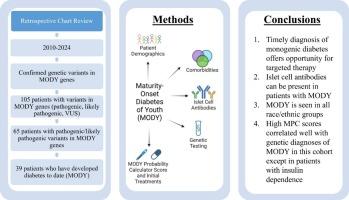
Methods
Retrospective chart review using MODY diagnoses and genetic testing was performed to identify patients with MODY gene variants at a large, pediatric tertiary referral center. Demographics, islet autoantibodies, and co-morbidities were evaluated with treatment change after diagnosis of MODY. Probability scores were calculated using the MPC.
Results
Thirty-nine patients were identified with MODY. MODY comprised 1 % of the population with diabetes. Mean age and HbA1c at diagnosis were 12.2 years and 7.9 %, respectively. Positive islet cell autoantibodies were seen in 2 individuals. For race, 23.1 % self-identified as Hispanic, Black, or Asian/Pacific Islander. Interestingly, 39.47 % did not require medication at diagnosis while 44.74 %, 10.53 %, and 2.63 % were treated with insulin, Metformin, and GLP-1 RA respectively. Seventy-four percent of patients with MODY had MPC scores of > 75 %. Targeted treatment with sulfonylureas was used for 38 % of total patients who remained on medication, and 20.5 % of patients were able to discontinue medication. Average HbA1c decreased for all patients with MODY regardless of medication treatment type at follow up.
Conclusions
Our data reveals that the presence of positive islet cell antibodies may not preclude a diagnosis of MODY if there is a strong clinical suspicion. High MPC scores correlated with diagnoses of MODY except in patients with insulin dependence. Diagnosis of MODY led to targeted treatment changes.
MODY的遗传变异和特征在一个单一的,大型儿科转诊中心
背景:由于治疗方法不同于其他形式的糖尿病,确定年轻人的成熟型糖尿病(MODY)至关重要。评估MODY患者的临床特征和MODY概率计算器(MPC)评分。方法回顾性分析一家大型儿科三级转诊中心的MODY诊断和基因检测,以确定MODY基因变异患者。统计数据、胰岛自身抗体和合并症与诊断MODY后的治疗变化进行了评估。使用MPC计算概率分数。结果39例确诊为MODY。MODY占糖尿病患者总数的1%。诊断时的平均年龄和HbA1c分别为12.2岁和7.9%。2例胰岛细胞自身抗体阳性。在种族方面,23.1%的人认为自己是西班牙裔、黑人或亚洲/太平洋岛民。有趣的是,39.47%的患者在诊断时不需要药物治疗,而分别有44.74%、10.53%和2.63%的患者接受了胰岛素、二甲双胍和GLP-1 RA治疗。74%的MODY患者MPC评分为>;75%。38%仍在用药的患者使用了磺脲类靶向治疗,20.5%的患者能够停药。在随访中,所有MODY患者的平均HbA1c均下降,无论药物治疗类型如何。结论sour数据显示,如果有强烈的临床怀疑,胰岛细胞抗体阳性可能不排除MODY的诊断。高MPC评分与MODY诊断相关,但胰岛素依赖患者除外。MODY的诊断导致了靶向治疗的改变。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Clinical and Translational Endocrinology
ENDOCRINOLOGY & METABOLISM-
CiteScore
6.10
自引率
0.00%
发文量
24
审稿时长
16 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


