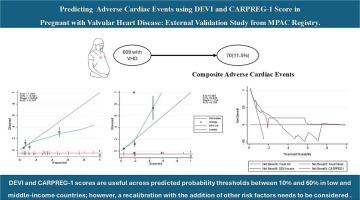
Predicting adverse cardiac events using DEVI and CARPREG-I score in pregnant with valvular heart disease: External validation study from MPAC registry
IF 2.6
3区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
While numerous risk assessment tools exist for pregnant women with valvular heart disease (VHD), validation studies assessing their performance in diverse settings are few. Such validation is crucial before applying these tools routinely in clinical practice.
Objectives
To validate and establish the clinical utility of two risk stratification tools – DEVI (VHD-specific tool) and CARPREG-I in predicting adverse cardiac events in pregnant women with VHD.
Methods
This cohort study involved consecutive pregnancies complicated with VHD enrolled in the prospective Medical College Pregnancy and Cardiac (MPAC) registry from July 2016 to December 2019. Individual risk for adverse composite cardiac events was calculated using DEVI and CARPREG-I models. Performance was assessed through discrimination and calibration characteristics. Clinical utility was evaluated with decision curve analysis.
Results
Of the 1029 pregnancies, 609 had VHD. Mitral regurgitation (67.2 %; 409/609) was most common; 11.5 % (70/609) experienced at least one component of the composite outcome. The area under the receiver operating characteristic curve was 0.747, with 95 % confidence intervals (CI) (0.685–0.809) for DEVI and 0.705 (95%CI 0.646–0.765) for CARPREG-I models. Calibration plots suggested that the DEVI score overestimates risk at higher probabilities, while the CARPREG-I score underestimates risk at most probabilities. Decision curve analysis demonstrated that both models were useful across predicted probability thresholds between 10 % and 60 %.
Conclusion
In this external validation study in pregnant women with VHD, both DEVI and CARPREG-I scores showed good discriminative ability and clinical utility across various probabilities. However, both models need recalibration to improve the agreement between the predicted and observed events.
使用DEVI和CARPREG-I评分预测瓣膜性心脏病孕妇的不良心脏事件:来自MPAC注册的外部验证研究
背景:虽然有许多风险评估工具存在于患有瓣膜性心脏病(VHD)的孕妇,但评估其在不同环境下表现的验证性研究很少。在将这些工具常规应用于临床实践之前,这种验证是至关重要的。目的:验证和建立两种风险分层工具——DEVI (VHD特异性工具)和CARPREG-I在预测VHD孕妇不良心脏事件中的临床应用。方法:本队列研究纳入了2016年7月至2019年12月在前瞻性医学院妊娠与心脏(MPAC)登记处登记的连续妊娠合并VHD患者。使用DEVI和CARPREG-I模型计算不良复合心脏事件的个体风险。通过判别和校准特性来评估性能。采用决策曲线分析评价临床疗效。结果:1029例妊娠中,609例发生VHD。二尖瓣返流(67.2% %;409/609)最为常见;11.0 %(70/609)至少经历了复合结局的一个组成部分。受试者工作特征曲线下面积为0.747,DEVI模型的置信区间为95 (0.685-0.809),CARPREG-I模型的置信区间为0.705 (95%CI 0.646-0.765)。校正图显示,DEVI评分在较高概率下高估了风险,而CARPREG-I评分在大多数概率下低估了风险。决策曲线分析表明,两种模型在预测概率阈值10 %和60 %之间都是有用的。结论:在这项针对VHD孕妇的外部验证研究中,DEVI和CARPREG-I评分在各种概率下都显示出良好的判别能力和临床实用性。然而,这两个模型都需要重新校准,以提高预测和观测事件之间的一致性。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Journal of cardiology
CARDIAC & CARDIOVASCULAR SYSTEMS-
CiteScore
4.90
自引率
8.00%
发文量
202
审稿时长
29 days
期刊介绍:
The official journal of the Japanese College of Cardiology is an international, English language, peer-reviewed journal publishing the latest findings in cardiovascular medicine. Journal of Cardiology (JC) aims to publish the highest-quality material covering original basic and clinical research on all aspects of cardiovascular disease. Topics covered include ischemic heart disease, cardiomyopathy, valvular heart disease, vascular disease, hypertension, arrhythmia, congenital heart disease, pharmacological and non-pharmacological treatment, new diagnostic techniques, and cardiovascular imaging. JC also publishes a selection of review articles, clinical trials, short communications, and important messages and letters to the editor.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


