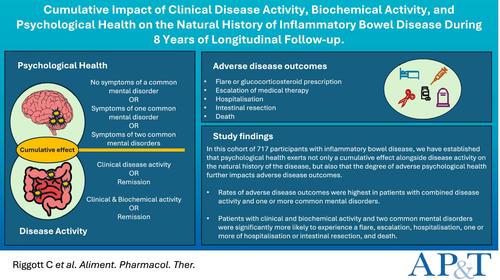
Cumulative Impact of Clinical Disease Activity, Biochemical Activity and Psychological Health on the Natural History of Inflammatory Bowel Disease During 8 Years of Longitudinal Follow-Up
Abstract
Background
Common mental disorders, including anxiety and depression, are prevalent in patients with inflammatory bowel disease (IBD) and may be associated with adverse outcomes. However, whether increasing psychological co-morbidity, in combination with disease activity, exerts a cumulative effect on prognosis is uncertain.
Aims
To assess this in a longitudinal follow-up study.
Methods
We collected baseline demographic and IBD-related information, clinical activity using disease activity scores and biochemical activity using calprotectin. Patients were grouped according to the presence or absence of disease activity. Patients in remission or with active disease were subgrouped according to the presence or absence of symptoms of a common mental disorder at baseline. We recorded the occurrence of adverse outcomes over 8.1 years, comparing their occurrence across subgroups using Cox regression.
Results
Among 717 participants with clinical activity data and 187 with clinical and biochemical activity data, rates of adverse outcomes increased with both disease activity and increasing psychological co-morbidity. Rates of flare or glucocorticosteroid prescription, escalation or death were higher with clinical activity (HR 2.89; 95% CI 1.68–4.93 and 2.52; 95% CI 1.55–4.10 and 6.97; 95% CI 2.43–20.0, respectively) or clinical and biochemical activity (HR 7.26; 95% CI 2.86–18.5, 3.62; 95% CI 1.59–8.25 and 57.3; 95% CI 7.58–433, respectively) and two common mental disorders. Rates of hospitalisation (HR 6.20; 95% CI 1.88–20.4) or hospitalisation and/or intestinal resection (HR 7.46; 95% CI 2.41–23.2) were higher with clinical and biochemical activity and two common mental disorders.
Conclusion
Psychological co-morbidity and active disease have a cumulative adverse impact on IBD prognosis.


 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


