Value of non-invasive test dynamics in guiding HCC surveillance decisions after HCV cure in patients with cirrhosis
IF 26.8
1区 医学
Q1 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
Abstract
Background and aims
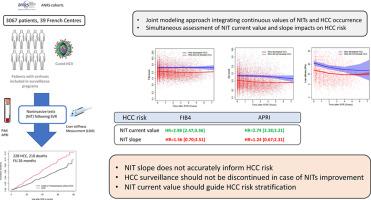
The objective was to describe the dynamics of noninvasive tests (NITs) in cirrhotic patients following sustained virological response (SVR) and to assess their correlation with hepatocellular carcinoma (HCC) risk.Methods
The dynamics of NITs (Fib4, APRI and LSM) were described in patients with cirrhosis after SVR included between 2006 and 2015 in two prospective French multicentre cohorts (ANRS CO22 Hepather and CO12 CirVir). To assess their relationship with the risk of HCC, a joint modeling approach was employed using both standard and flexible models adjusted for age and sex. The impacts of NIT current value and slope during follow-up on HCC risk were assessed taking into account competing risks of death.Results
3067 patients with cirrhosis who achieved SVR were analyzed, among whom 228 (7.4%) developed HCC and 210 (6.9%) died during a 26-month follow-up. All NITs were increased at baseline in patients who ultimately developed HCC, whereas platelet counts were lower. All NITs improved in patients who did not develop HCC. More contrasted changes were observed during the follow-up of patients who ultimately developed HCC. Joint model analyses showed that current values of Fib4, APRI and platelet count at any time impacted HCC risk. Only Fib4 and APRI slopes influenced the same outcome. When considering NIT current value and slope simultaneously, only the current value of NITs impacted HCC risk while the slopes were not informative.Conclusions
The dynamics of NITs following SVR do not identify cirrhotic patients who could be safely excluded from surveillance programmes. NIT current value is more informative than slope which would necessitate to regularly re-assess HCC risk to design individualized surveillance strategies.Impact and implications
It has been postulated that that monitoring noninvasive tests (NIT) dynamics following HCV cure may inform on HCC residual risk in patients with cirrhosis, and may allow for the discontinuation of surveillance in certain patient subsets. We analyzed data from over 3,000 patients and found that while all NITs improved in cirrhotic patients who did not develop HCC, those who eventually developed liver cancer showed more contrasted changes in these tests. Specifically, the current values of tests like Fib4 and APRI were linked to an increased risk of HCC. while their slopes did not provide additional useful information, suggesting that dedicated prospective studies are warranted to define how repeated measurement of NIT could be combined with other variables into HCC risk stratification algorithms. Until then, HCC surveillance should be maintained in all patients with cirrhosis following HCV eradication, even in case of decreased NIT.
无创检测动态在指导肝硬化患者HCV治愈后HCC监测决策中的价值
背景和目的目的是描述持续病毒学反应(SVR)后肝硬化患者无创检查(NITs)的动态,并评估其与肝细胞癌(HCC)风险的相关性。方法:在2006年至2015年间纳入两个前瞻性法国多中心队列(ANRS CO22 Hepather和CO12 CirVir)的SVR后肝硬化患者中,描述了NITs (fifi4、APRI和LSM)的动态。为了评估它们与HCC风险的关系,采用了一种联合建模方法,使用标准模型和根据年龄和性别调整的灵活模型。在考虑竞争死亡风险的情况下,评估随访期间NIT现值和斜率对HCC风险的影响。结果分析3067例达到SVR的肝硬化患者,其中228例(7.4%)发生HCC, 210例(6.9%)在26个月的随访期间死亡。在最终发展为HCC的患者中,所有nit在基线时均升高,而血小板计数较低。未发生HCC的患者的NITs均有改善。在最终发展为HCC的患者随访期间观察到更多的对比变化。联合模型分析显示,任何时候Fib4、APRI和血小板计数的当前值都会影响HCC的风险。只有Fib4和APRI斜率影响相同的结果。当同时考虑NIT电流值和斜率时,只有NIT电流值影响HCC风险,而斜率没有信息。结论:SVR后的NITs动态并不能确定哪些肝硬化患者可以安全地排除在监测计划之外。NIT的现值比斜率更能提供信息,因此有必要定期重新评估HCC风险,以设计个性化的监测策略。影响和意义有假设认为,监测HCV治愈后的无创检测(NIT)动态可以告知肝硬化患者的HCC残留风险,并可能允许在某些患者亚群中停止监测。我们分析了来自3000多名患者的数据,发现虽然未发展为HCC的肝硬化患者的所有nit都有所改善,但最终发展为肝癌的患者在这些测试中表现出更多的对比变化。具体来说,目前的检测值如Fib4和APRI与HCC的风险增加有关。而他们的斜率并没有提供额外的有用信息,这表明有必要进行专门的前瞻性研究,以确定如何将NIT的重复测量与其他变量结合到HCC风险分层算法中。在此之前,即使在NIT下降的情况下,所有HCV根除后肝硬化患者仍应保持HCC监测。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Hepatology
医学-胃肠肝病学
CiteScore
46.10
自引率
4.30%
发文量
2325
审稿时长
30 days
期刊介绍:
The Journal of Hepatology is the official publication of the European Association for the Study of the Liver (EASL). It is dedicated to presenting clinical and basic research in the field of hepatology through original papers, reviews, case reports, and letters to the Editor. The Journal is published in English and may consider supplements that pass an editorial review.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


