The health and economic burden of brain disorders: Consequences for investment in diagnosis, treatment, prevention and R&D
IF 2.8
Q3 CLINICAL NEUROLOGY
引用次数: 0
Abstract
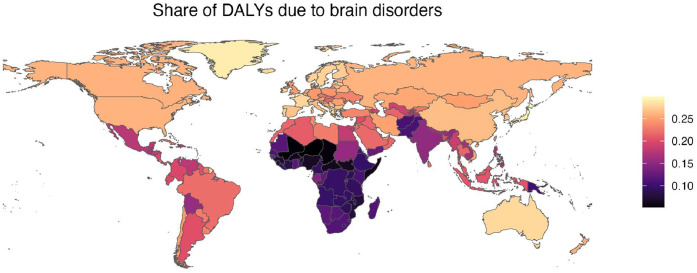
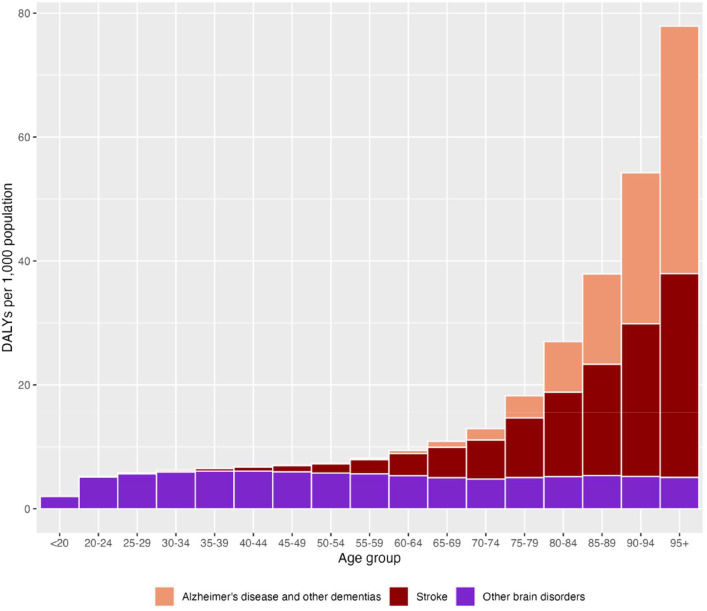
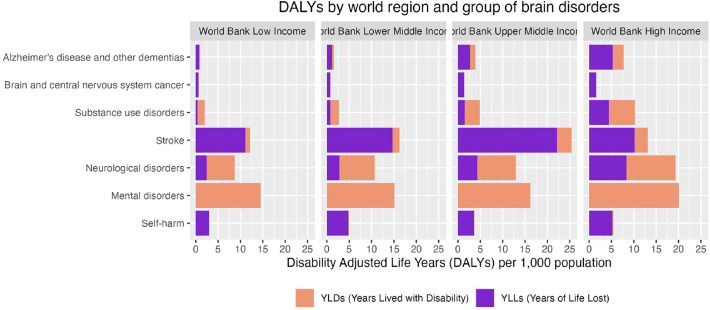
Brain disorders are prevalent across all age groups but particularly in the elderly, highlighting the importance of preserving brain health in ageing populations. There have been few previous studies to address the complete scope of burden of brain disorders, including direct and indirect costs as well as intangible costs from morbidity and mortality. We seek to illustrate the full health and economic impact of brain disorders by leveraging data from previous large-scale epidemiological and health economic studies to estimate the total direct, indirect and intangible cost of brain disorders in 2019. Two alternative methods were used to estimate indirect costs: the human capital (HC) method (data from the CBDE2010 study), and the willingness-to-pay (WTP) per DALY method (data from GBD2019). Less than 10% of the costs of Alzheimer's disease (AD) and other dementias are incurred by the health care system, while Alzheimer's disease and other dementias is the costliest condition using the HC approach and stroke is the costliest condition due to the large number of life-years lost, followed by AD using the WTP approach. Using per-capita GDP as a proxy for WTP, the indirect costs were nearly four times higher compared to the conventional HC approach. We found that Indirect costs of brain disorders outweigh the direct costs for diagnosis, treatment and care even in high-income countries with advanced, universally accessible systems in Europe. There is likely underinvestment in R&D for brain disorders, and health care systems may lack sufficient incentives to invest in their treatment and prevention.
脑部疾病的健康和经济负担:诊断、治疗、预防和研发投资的后果。
脑部疾病在所有年龄组中都很普遍,但在老年人中尤为普遍,这凸显了在老龄人口中保持脑部健康的重要性。以前很少有研究涉及脑部疾病负担的全部范围,包括直接和间接成本以及发病率和死亡率的无形成本。我们试图利用以往大规模流行病学和卫生经济学研究的数据来估计2019年脑部疾病的直接、间接和无形总成本,从而说明脑部疾病对健康和经济的全面影响。使用了两种替代方法来估算间接成本:人力资本(HC)方法(来自CBDE2010研究的数据)和每个DALY的支付意愿(WTP)方法(来自GBD2019的数据)。不到10%的阿尔茨海默病(AD)和其他痴呆症的费用是由卫生保健系统产生的,而阿尔茨海默病和其他痴呆症是使用HC方法成本最高的疾病,中风是成本最高的疾病,因为损失了大量的生命年,其次是使用WTP方法的AD。使用人均GDP作为WTP的代表,间接成本比传统的HC方法高出近四倍。我们发现,脑部疾病的间接成本超过了诊断、治疗和护理的直接成本,即使在欧洲拥有先进、普遍可及系统的高收入国家也是如此。对脑部疾病的研发投资可能不足,卫生保健系统可能缺乏足够的激励来投资于脑部疾病的治疗和预防。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Cerebral circulation - cognition and behavior
Neurology, Clinical Neurology
CiteScore
2.00
自引率
0.00%
发文量
0
审稿时长
14 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


