Testicular function in postpubertal patients with growth hormone deficiency: A prospective controlled study
IF 3.3
Q1 ENDOCRINOLOGY & METABOLISM
Journal of Clinical and Translational Endocrinology
Pub Date : 2025-01-15
DOI:10.1016/j.jcte.2025.100383
引用次数: 0
Abstract
Background
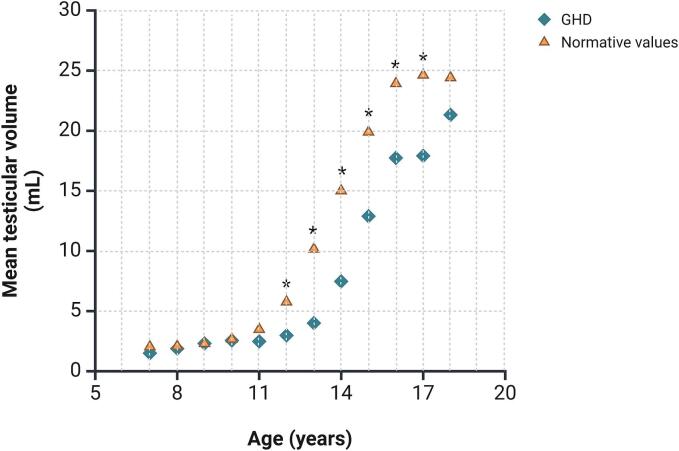
We have previously shown that treatment with recombinant human growth hormone (GH) influences testicular growth in children with GH deficiency (GHD) and have suggested that GH plays a role in testicular growth in childhood. Little evidence is available on testicular function in post-pubertal GHD patients.
Objective
This prospective controlled study was undertaken to evaluate testicular function in patients with GHD.
Patients and Methods
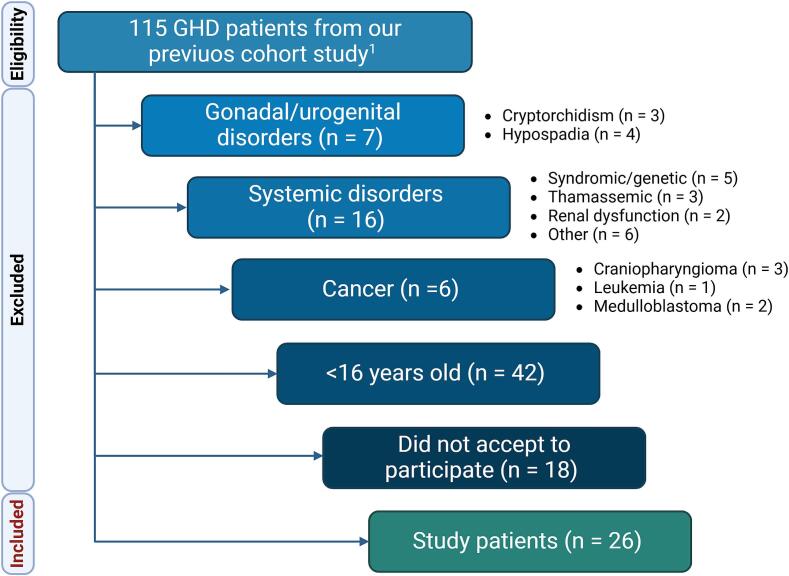
Post-pubertal patients with non-syndromic GHD over the age of 16 years were enrolled. Each patient underwent to the assessment of serum levels of gonadotropins and total testosterone (TT), conventional sperm parameters, and testicular volume (TV) measured by ultrasound examination. Age-matched healthy subjects served as controls. Patients with disorders capable of interfering with testicular function were excluded.
Results
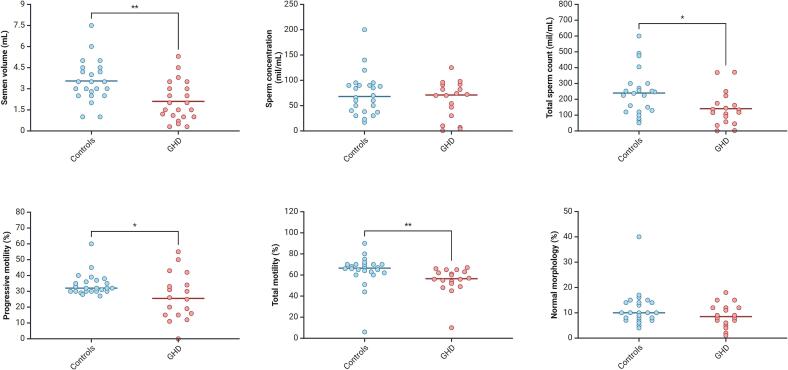
26 patients with GHD and 25 age-matched post-pubertal controls were enrolled. They did not differ in serum luteinizing hormone, follicle-stimulating hormone, and TT levels. However, GHD patients had lower semen volume, total sperm count, progressive motility, and total motility values, and a higher prevalence of oligozoospermia compared to controls. No difference was found in sperm concentration and normal morphology. Importantly, GHD patients had lower TV, and a higher prevalence of testicular hypotrophy.
Conclusion
This is the first evidence of mildly impaired sperm parameters and TV in GHD patients compared to healthy controls. The integrity of the GH-IGF1 axis in prepuberty is important for achieving normal testicular function in adulthood. Evaluating testicular growth over time in GHD children and measuring TV and sperm parameters in postpubertal GHD boys is advisable.
青春期后生长激素缺乏患者的睾丸功能:一项前瞻性对照研究。
背景:我们之前已经表明,重组人生长激素(GH)治疗会影响GH缺乏症(GHD)儿童的睾丸生长,并提示GH在儿童睾丸生长中起作用。关于青春期后GHD患者睾丸功能的证据很少。目的:本前瞻性对照研究旨在评估GHD患者的睾丸功能。患者和方法:入选年龄在16岁以上的青春期后非综合征性GHD患者。对患者进行血清促性腺激素和总睾酮水平(TT)、常规精子参数和超声测量睾丸体积(TV)的评估。年龄匹配的健康受试者作为对照。排除有干扰睾丸功能障碍的患者。结果:纳入了26例GHD患者和25例年龄匹配的青春期后对照。他们在血清促黄体生成素、促卵泡激素和TT水平上没有差异。然而,与对照组相比,GHD患者的精液量、精子总数、进行性活动力和总活动力值较低,少精症的患病率较高。精子浓度和正常形态无差异。重要的是,GHD患者的TV较低,睾丸功能减退的患病率较高。结论:与健康对照相比,这是GHD患者精子参数和TV轻度受损的第一个证据。青春期前GH-IGF1轴的完整性对于成年后实现正常睾丸功能至关重要。建议评估GHD儿童睾丸随时间的生长情况,并测量青春期后GHD男孩的TV和精子参数。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Clinical and Translational Endocrinology
ENDOCRINOLOGY & METABOLISM-
CiteScore
6.10
自引率
0.00%
发文量
24
审稿时长
16 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


