Successful Treatment of Benign Insulinoma by Transcatheter Angioembolization
IF 1.2
Q3 Medicine
引用次数: 0
Abstract
Background/Objective
Evidence on the efficacy and safety of minimally invasive treatment for insulinoma has increased over the past decade to the point of becoming a recommendation in clinical practice guidelines for the management of this type of neuroendocrine tumor.
Case Report
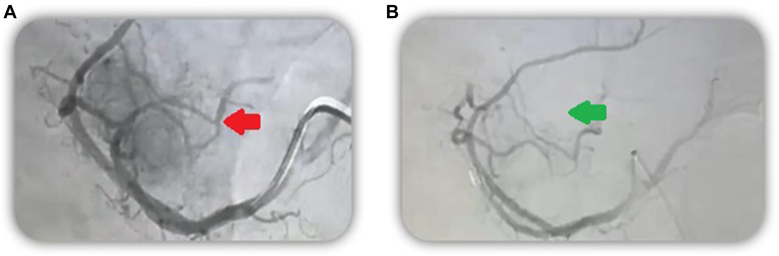
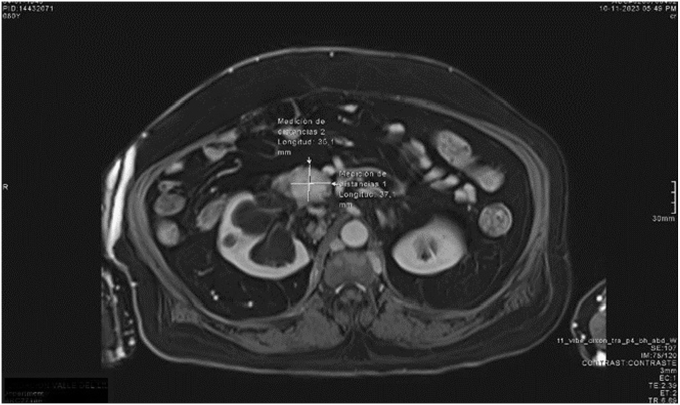
We describe the case of an elderly male patient with multiple comorbidities and recurrent isolated insulinoma of 3.7 × 3.5 cm involving the uncinate process of the pancreas and contacting the splenomesenteric confluent many years after first resection, in whom, after refusing surgical management, was performed as successful arterial embolization of the pancreatic tumor.
Discussion
When addressing this pathology, it is common to encounter patients who are not candidates for surgical management, either due to the presence of comorbidities, the location of the tumor in relation to vascular structures, or refusal of the intervention. Therefore, it is important to be aware of the different therapeutic options in localized and metastatic disease.
Conclusion
Minimally invasive procedures are positioned as an effective alternative for the treatment of the hormonal overproduction in patients with insulinoma.
经导管血管栓塞成功治疗良性胰岛素瘤。
背景/目的:在过去的十年中,关于胰岛素瘤微创治疗的有效性和安全性的证据越来越多,已经成为治疗这类神经内分泌肿瘤的临床实践指南的推荐。病例报告:我们描述了一例老年男性患者,在首次切除多年后,患有多种合并症和复发的3.7 × 3.5 cm的孤立胰岛素瘤,累及胰腺棘突并接触脾肠系膜汇合处,在拒绝手术治疗后,成功地对胰腺肿瘤进行了动脉栓塞。讨论:在处理这种病理时,通常会遇到不适合手术治疗的患者,或者是由于合并症的存在,肿瘤与血管结构的关系,或者是拒绝干预。因此,了解局部和转移性疾病的不同治疗选择是很重要的。结论:微创手术是治疗胰岛素瘤患者激素分泌过多的有效选择。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

AACE Clinical Case Reports
Medicine-Endocrinology, Diabetes and Metabolism
CiteScore
2.30
自引率
0.00%
发文量
61
审稿时长
55 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


