Uremic Leontiasis Ossea due to Resistant Secondary Hyperparathyroidism
IF 1.2
Q3 Medicine
引用次数: 0
Abstract
Background/Objective
Severe progressive overgrowth of the facial bones known as uremic leontiasis ossea (ULO) is a rare complication of resistant hyperparathyroidism in end-stage renal disease (ESRD). The objective of this report is to describe the presentation and treatment of ULO.
Case Report
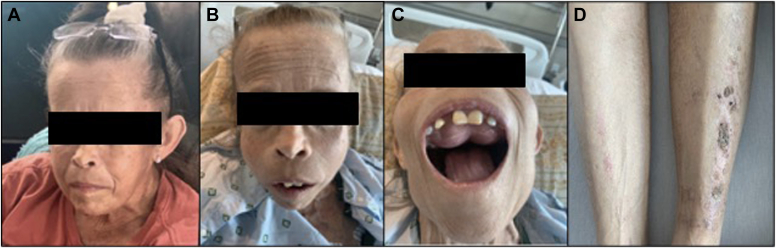
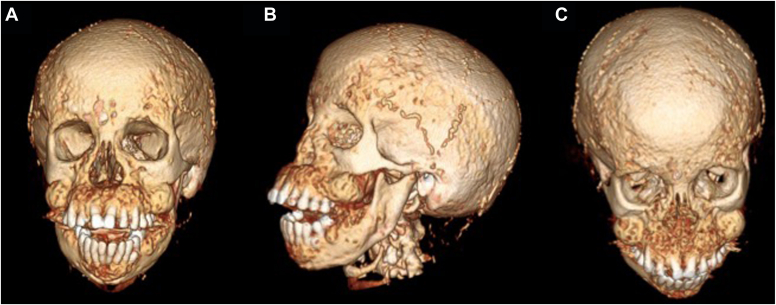
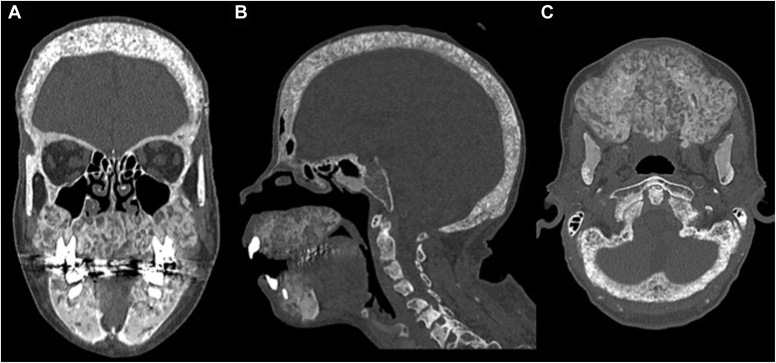
A 48-year-old woman with a history of hypertension, coronary artery disease, and ESRD on hemodialysis presented with severe secondary hyperparathyroidism and calciphylaxis. She had significant changes to her face in the last 3 months leading to oropharyngeal dysphagia and difficulty articulating. Physical examination revealed bony overgrowth in her upper jaw and hard palate, widely spaced teeth, and calcinosis cutis. Her parathyroid hormone (PTH), calcium, and phosphorus levels were 5066 pg/mL (normal range, 12-88 pg/mL); 10.0 mg/dL (8.4-10.2 mg/dL); and 5.4 mg/dL (2.7-4.5 mg/dL); respectively. Using a multidisciplinary approach, she successfully underwent a 3.5-gland parathyroidectomy (immediate postoperative PTH level, 600 pg/mL). She was discharged without complication. Pathology showed hypercellular parathyroid glands with reactive changes.
Discussion
ULO, the most severe form of renal osteodystrophy, results in hypertrophy of the craniofacial skeleton. It carries the risk of significant comorbidities due to cranial nerve compression, respiratory compromise, dysarthria, and dysphagia.
Conclusion
With prolonged, uncontrolled PTH stimulation in ESRD, significant facial disfiguration with disabilities can occur. It is of utmost importance to adhere to guideline-specified PTH targets in persons with ESRD to prevent patient harm from permanent physical deformities.
顽固性继发性甲状旁腺功能亢进所致的骨质疏松性尿毒症。
背景/目的:骨性尿毒症(ULO)是终末期肾脏疾病(ESRD)中难治性甲状旁腺功能亢进的罕见并发症。本报告的目的是描述ULO的表现和治疗。病例报告:一名48岁女性,有高血压、冠状动脉疾病和ESRD的血液透析史,表现为严重的继发性甲状旁腺功能亢进和钙化反应。在过去的3个月里,她的面部发生了明显的变化,导致口咽吞咽困难和发音困难。体格检查发现她的上颚和硬腭骨质增生,牙齿间距大,皮肤钙质沉着。甲状旁腺激素(PTH)、钙、磷水平5066 pg/mL(正常范围12-88 pg/mL);10.0 mg/dL (8.4-10.2 mg/dL);和5.4 mg/dL (2.7-4.5 mg/dL);分别。采用多学科方法,她成功地接受了3.5腺甲状旁腺切除术(术后立即PTH水平为600 pg/mL)。她出院了,没有并发症。病理表现为甲状旁腺细胞增生伴反应性改变。讨论:ULO是肾性骨营养不良最严重的形式,导致颅面骨骼肥大。由于颅神经压迫、呼吸损害、构音障碍和吞咽困难,它具有显著合并症的风险。结论:在ESRD中,长时间不受控制的甲状旁腺激素刺激可导致明显的面部畸形和残疾。在ESRD患者中,坚持指南规定的PTH目标以防止患者遭受永久性身体畸形的伤害是至关重要的。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

AACE Clinical Case Reports
Medicine-Endocrinology, Diabetes and Metabolism
CiteScore
2.30
自引率
0.00%
发文量
61
审稿时长
55 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


