Anemia in diabetes mellitus: Pathogenetic aspects and the value of early erythropoietin therapy
IF 2.7
引用次数: 0
Abstract
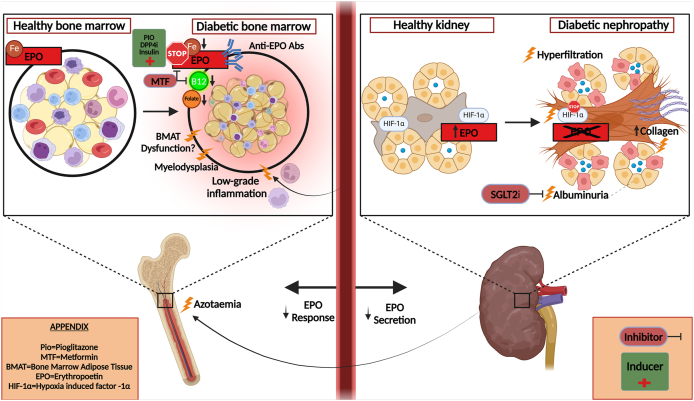
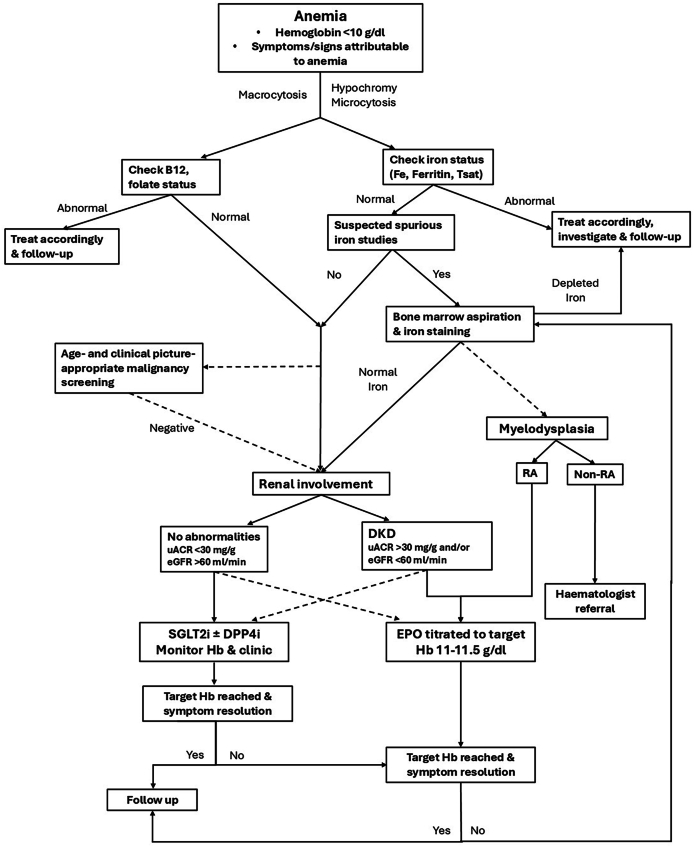
Anemia is a frequent, yet increasingly recognized, comorbidity in diabetes mellitus (DM), with prevalence often driven by multifactorial mechanisms. Hematinic deficiencies, common in this population, may arise from associated comorbidities or medications, such as metformin, as well as other drugs commonly employed for DM-related conditions. Among contributing factors, diabetic kidney disease (DKD) plays a pivotal role, with anemia developing more frequently and being more pronounced in earlier stages, than in CKD of other causes. This enhanced susceptibility stems primarily from the combined impact of impaired renal oxygen sensing and deficient erythropoietin (EPO) production linked to tubulointerstitial fibrosis. Additional mechanisms comprise glomerular dysfunction, shortened erythrocyte lifespan, uremia-induced bone marrow suppression, and increased bleeding risk. DM is also recognized as a chronic low-grade inflammatory condition, with its inflammatory burden driving iron maldistribution, suppression of erythropoiesis, and resistance to EPO. The diagnostic approach of anemia in DM mirrors that in the general population. Addressing modifiable causes such as hematinic deficiencies, and other chronic conditions, such as DKD and bone marrow disorders, is paramount. In total, the underlying pathophysiology of anemia in DM primarily reflects a state of absolute or relative EPO deficiency and/or diminished bone marrow responsiveness, effectively corresponding to 'anemia of chronic disease. Early initiation of EPO therapy, even in DM patients without overt DKD, may mitigate disease progression and improve outcomes. Future research should focus on diabetes-specific strategies integrating optimal EPO use, potentially implementing targeted management of renal and inflammatory contributors to anemia.
糖尿病贫血:发病方面和早期促红细胞生成素治疗的价值。
贫血是糖尿病(DM)中一种常见的合并症,但越来越多的人认识到,其患病率通常由多因素机制驱动。在这一人群中常见的血液学缺陷可能是由相关的合并症或药物引起的,如二甲双胍,以及其他通常用于dm相关疾病的药物。在这些因素中,糖尿病肾病(DKD)起着关键作用,与其他原因的CKD相比,贫血在早期阶段更频繁和更明显。这种增强的易感性主要源于肾氧感知受损和与小管间质纤维化相关的促红细胞生成素(EPO)产生不足的综合影响。其他机制包括肾小球功能障碍、红细胞寿命缩短、尿毒症诱导的骨髓抑制和出血风险增加。糖尿病也被认为是一种慢性低度炎症,其炎症负担导致铁分布失调,抑制红细胞生成,并对促红细胞生成素产生抵抗。糖尿病患者贫血的诊断方法与普通人群相同。解决可改变的原因,如血液病缺乏和其他慢性疾病,如DKD和骨髓疾病,是至关重要的。总的来说,糖尿病贫血的潜在病理生理主要反映了绝对或相对EPO缺乏和/或骨髓反应性降低的状态,有效地对应于“慢性疾病贫血”。即使在没有明显DKD的糖尿病患者中,早期开始EPO治疗也可能减缓疾病进展并改善预后。未来的研究应侧重于糖尿病特异性策略,整合最佳促红细胞生成素的使用,潜在地实施肾脏和炎症性贫血的靶向管理。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Metabolism open
Agricultural and Biological Sciences (General), Endocrinology, Endocrinology, Diabetes and Metabolism
自引率
0.00%
发文量
0
审稿时长
40 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


