A descriptive report on the impact of pharmacy workflows in the operational success of hospital at home implementation at a county academic hospital system
IF 1.8
Q3 PHARMACOLOGY & PHARMACY
Exploratory research in clinical and social pharmacy
Pub Date : 2025-01-04
DOI:10.1016/j.rcsop.2025.100560
引用次数: 0
Abstract
Background
The hospital at home (HaH) model has become more prevalent in the American healthcare system due to its ability to decrease acute care costs and readmission risk. Recent publications have provided guidance on optimizing medication management and patient safety by leveraging clinical pharmacy services. There is limited data on pharmacoeconomic impact of HaH implementation, specifically in underinsured patients.
Objective(s)
To describe the development of HaH-related pharmacy workflows and evaluate the operational success of the program in an underinsured patient population.
Methods
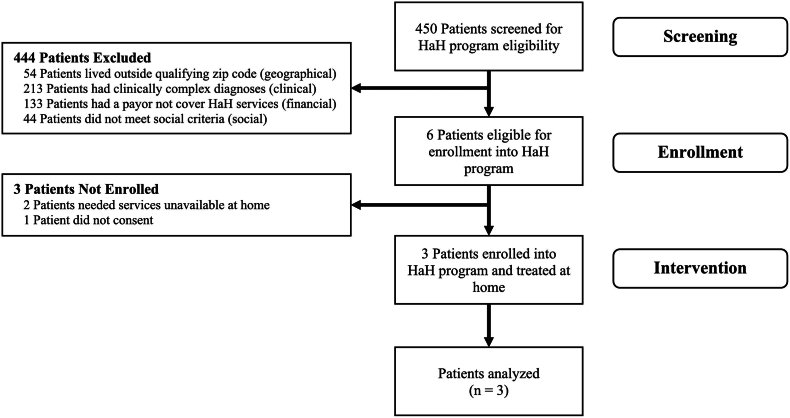
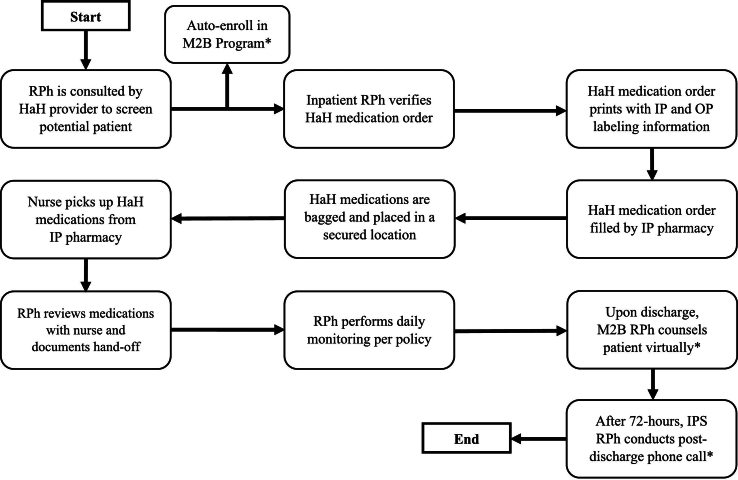
This report describes HaH program implementation between August 1st, 2022, and March 19th, 2024. Patients were eligible for home treatment if they met geographic, clinical, financial, and social criteria.
Outcomes
The primary outcome measured was the quantity and cost of medication waste for patients treated at home. Secondary outcomes included HaH medication turnaround time, healthcare resource utilization, and patient safety. All study outcomes were reported using descriptive statistics.
Results
Out of 450 patients screened, 3 met criteria and provided consent for HaH enrollment. The total cost of medication waste for all 3 patients was $41.15, and 21 out of 53 dispensed doses (40 %) were wasted. The mean medication verification time was 8.1 min, and the mean medication preparation time was 50.2 min.
Conclusion
Study data provides insight into enhancing dispensing practices while establishing the benefits pharmacists bring to the HaH care team. Future research should elaborate on other measures of operational success to identify optimal performance metrics to support expanding pharmaceutical services within the HaH care model.
一份关于药房工作流程对县学术医院系统居家医院实施成功的影响的描述性报告。
背景:家庭医院(HaH)模式在美国医疗保健系统中变得越来越普遍,因为它能够降低急性护理成本和再入院风险。最近的出版物提供了通过利用临床药学服务来优化药物管理和患者安全的指导。关于实施HaH的药物经济学影响的数据有限,特别是在保险不足的患者中。目的:描述与哈氏病相关的药房工作流程的发展,并评估该计划在保险不足的患者群体中的运作成功。方法:本报告描述了2022年8月1日至2024年3月19日期间的ha计划实施情况。如果患者符合地理、临床、经济和社会标准,他们就有资格接受家庭治疗。结果:测量的主要结果是在家治疗的患者的药物浪费的数量和成本。次要结果包括HaH药物周转时间、医疗资源利用率和患者安全。所有研究结果均采用描述性统计进行报告。结果:在筛选的450例患者中,有3例符合标准并同意加入HaH。所有3名患者的药物浪费总成本为41.15美元,53个分配剂量中有21个(40%)被浪费。平均药物验证时间为8.1 min,平均药物准备时间为50.2 min。结论:研究数据为加强调剂实践提供了见解,同时确立了药师为HaH护理团队带来的利益。未来的研究应详细阐述运营成功的其他措施,以确定最佳绩效指标,以支持在HaH护理模式内扩大药品服务。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Exploratory research in clinical and social pharmacy
Public Health and Health Policy
CiteScore
1.60
自引率
0.00%
发文量
0
审稿时长
103 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


