Influence of hydrocortisone infusion method on the clinical outcome of patients with septic shock: A systematic review and meta-analysis
引用次数: 0
Abstract
Background
The effect of the modality of hydrocortisone administration on clinical outcomes in patients with septic shock remains uncertain. This systematic review and meta-analysis evaluate the impact of intermittent bolus and continuous infusion of hydrocortisone on these outcomes.
Methods
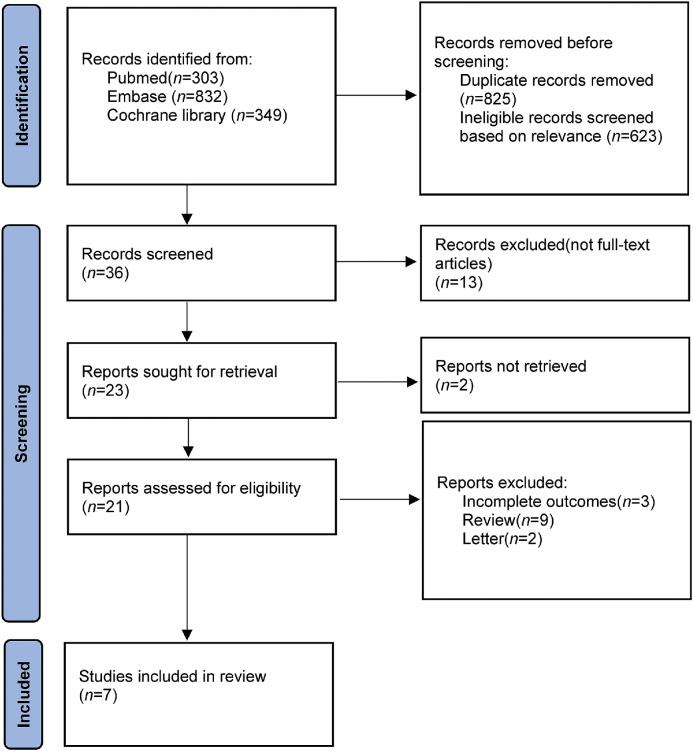
We searched the PubMed, Embase databases, and Cochrane Library for randomized controlled trials (RCTs) and cohort studies published from inception to January 1, 2023. We included studies involving adult patients with septic shock. All authors reported our primary outcome of short-term mortality and clearly compared the clinically relevant secondary outcomes (ICU length of stay, hospital length of stay, vasopressor-free days, hyperglycemia, hypernatremia, and ICU-acquired weakness [ICUAW]) of intermittent bolus and continuous infusion of hydrocortisone. Results were expressed as odds ratio (OR) and mean difference (MD) with accompanying 95% confidence interval (CI). The PROSPERO registration number is CRD42023392160.
Results
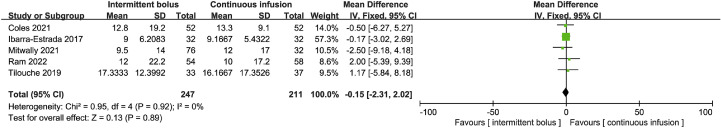
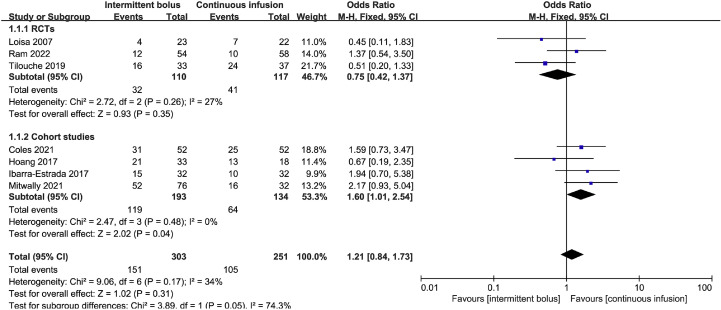
Seven studies, including 554 patients, were included. The primary outcome of this meta-analysis showed no statistically significant difference in the short-term mortality between intermittent bolus and continuous infusion groups (OR=1.21, 95% CI: 0.84 to 1.73; P=0.31; Chi2=9.06; I2=34%). Secondary outcomes showed no statistically significant difference in the ICU length of stay (MD=−0.15, 95% CI: −2.31 to 2.02; P=0.89; Chi2=0.95; I2=0%), hospital length of stay (MD=0.63, 95% CI: −4.24 to 5.50; P=0.80; Chi2=0.61; I2=0%), vasopressor-free days (MD=−1.18, 95% CI: −2.43 to 0.06; P=0.06; Chi2=2.48; I2=60%), hyperglycemia (OR=1.27, 95% CI: 0.80 to 2.02; P=0.31; Chi2=5.23; I2=43%), hypernatremia (OR=0.93, 95% CI: 0.44 to 1.96; P=0.85; Chi2=0.37; I2=0%), or ICUAW (OR=0.83, 95% CI: 0.36 to 1.94; P=0.67; Chi2=0.90; I2=0%) between the two groups.
Conclusions
This meta-analysis indicated no significant difference in short-term mortality between intermittent bolus or continuous hydrocortisone infusion in patients with septic shock. Additionally, the hydrocortisone infusion method was not associated with ICU length of stay, hospital length of stay, vasopressor-free days, hyperglycemia, hypernatremia, or ICUAW.
氢化可的松输注方式对脓毒性休克患者临床结局的影响:一项系统回顾和荟萃分析。
背景:氢化可的松给药方式对脓毒性休克患者临床结局的影响尚不确定。本系统综述和荟萃分析评估了间歇性注射和持续输注氢化可的松对这些结果的影响。方法:我们检索PubMed、Embase数据库和Cochrane图书馆,检索从成立到2023年1月1日发表的随机对照试验(rct)和队列研究。我们纳入了涉及感染性休克成年患者的研究。所有作者都报告了短期死亡率的主要结局,并明确比较了间歇输注和持续输注氢化可的松的临床相关次要结局(ICU住院时间、住院时间、无血管加压剂天数、高血糖、高钠血症和ICU获得性虚弱[ICUAW])。结果以比值比(OR)和平均差(MD)表示,并伴有95%置信区间(CI)。普洛斯彼罗注册号为CRD42023392160。结果:纳入7项研究,554例患者。该荟萃分析的主要结局显示,间歇输注组和持续输注组的短期死亡率无统计学差异(OR=1.21, 95% CI: 0.84 ~ 1.73;P = 0.31;Chi2 = 9.06;我2 = 34%)。次要结局显示ICU住院时间差异无统计学意义(MD=-0.15, 95% CI: -2.31 ~ 2.02;P = 0.89;Chi2 = 0.95;I 2=0%)、住院时间(MD=0.63, 95% CI: -4.24 ~ 5.50;P = 0.80;Chi2 = 0.61;I 2=0%),无血管加压剂天数(MD=-1.18, 95% CI: -2.43 ~ 0.06;P = 0.06;Chi2 = 2.48;I 2=60%),高血糖(OR=1.27, 95% CI: 0.80 ~ 2.02;P = 0.31;Chi2 = 5.23;I 2=43%)、高钠血症(OR=0.93, 95% CI: 0.44 ~ 1.96;P = 0.85;Chi2 = 0.37;I 2=0%)或ICUAW (or =0.83, 95% CI: 0.36 ~ 1.94;P = 0.67;Chi2 = 0.90;I 2=0%)。结论:该荟萃分析显示,间歇输注氢化可的松与持续输注氢化可的松在感染性休克患者的短期死亡率无显著差异。此外,氢化可的松输注方法与ICU住院时间、住院时间、无血管加压剂天数、高血糖、高钠血症或ICUAW无关。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of intensive medicine
Critical Care and Intensive Care Medicine
CiteScore
1.90
自引率
0.00%
发文量
0
审稿时长
58 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


