Awake prone positioning and ventilation distribution as assessed by electric impedance tomography in patients with non-COVID-19 acute hypoxemic respiratory failure: A prospective physiology study
引用次数: 0
Abstract
Background
Awake prone positioning (APP) can reportedly reduce the need for intubation and help improve prognosis of patients with acute hypoxemic respiratory failure (AHRF) infected with COVID-19. However, its physiological mechanism remains unclear. In this study, we evaluated the effect of APP on lung ventilation in patients with moderate-to-severe AHRF to better understand the effects on ventilation distribution and to prevent intubation in non-intubated patients.
Methods
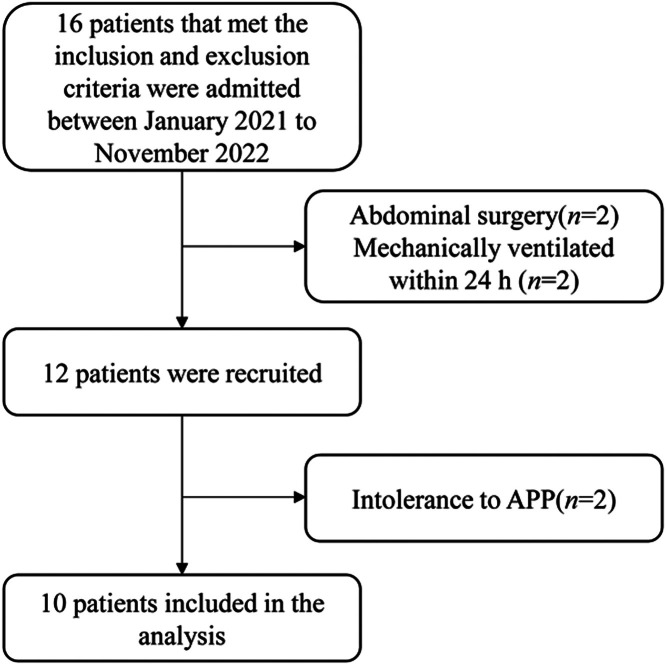
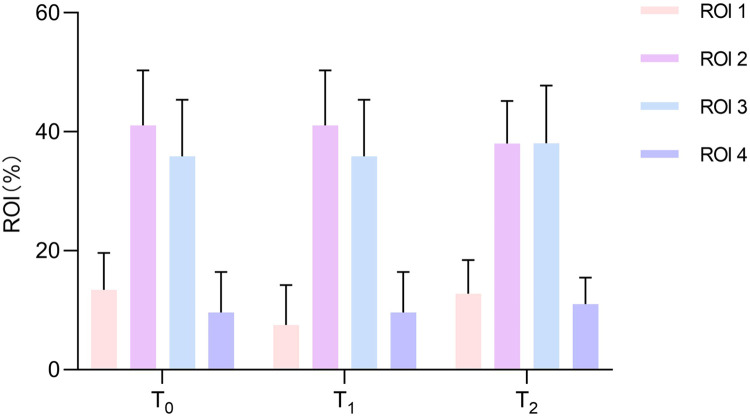
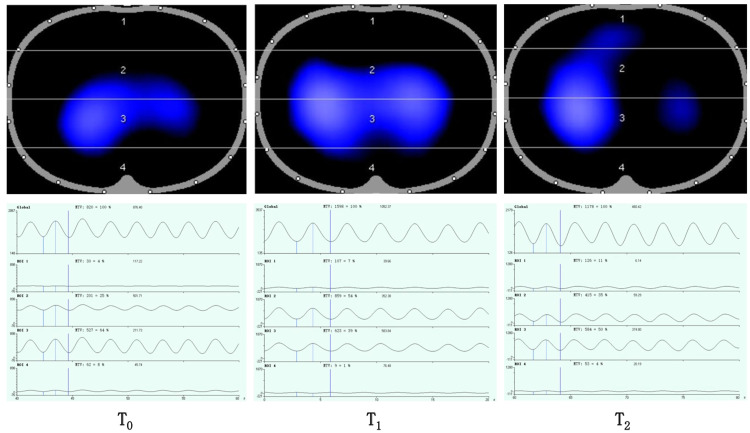
The prospective study was performed in the Department of Critical Care Medicine at Shanghai General Hospital, China, from January 2021 to November 2022. The study included patients with AHRF (partial pressure of oxygen [PaO2]/inspired oxygen concentration [FiO2] <200 mmHg or oxygen saturation [SpO2]/FiO2 <235) treated with high-flow nasal oxygen. Electrical impedance tomography (EIT) measurements including center of ventilation (COV), global inhomogeneity (GI) index, and regional ventilation delay (RVD) index were performed in the supine position (T0), 30 min after the start of APP (T1), and 30 min returning to supine position after the APP (T2). Clinical parameters like SpO2, respiratory rate (RR), FiO2, heart rate (HR), and ROX (the ratio of SpO2 as measured by pulse oximetry/FiO2 to RR) were also recorded simultaneously at T0, T1, and T2. To evaluate the effect of the time points on the variables, Mauchly's test was performed for sphericity and repeated measures analysis of variance was applied with Bonferroni's post hoc multiple comparisons.
Results
Ten patients were enrolled. The PaO2/FiO2 ratio was (111.4±33.4) mmHg at the time of recruitment. ROX showed a significant increase after initiation of APP {median (interquartile range [IQR]): T0: 7.5 (6.0–10.1) vs. T1: 7.6 (6.4–9.3) vs. T2: 8.3 (7.2–11.0), P=0.043}. RR (P=0.409), HR (P=0.417), and SpO2/FiO2 (P=0.262) did not change significantly during prone positioning (PP). The COV moved from the ventral area to the dorsal area (T0: 48.8%±6.2% vs. T1: 54.8%±6.8% vs. T2: 50.3%±6.1%, P=0.030) after APP. The GI decreased significantly after APP (T0: median=42.7 %, [IQR: 38.3%–47.5%] vs. T1: median=38.2%, [IQR: 34.6%–50.7%] vs. T2: median=37.4%, [IQR: 34.2%–41.4%], P=0.049). RVD (P=0.794) did not change after APP.
Conclusions
APP can improve ventilation distribution and homogeneity of lung ventilation as assessed by EIT in non-intubated patients with AHRF.
Trail Registration Chinese Clinical Trial Registry Identifier: ChiCTR2000035895.
电阻抗断层成像评估非covid -19急性低氧性呼吸衰竭患者清醒俯卧位和通气分布:一项前瞻性生理学研究
背景:据报道,清醒俯卧位(APP)可以减少COVID-19感染的急性低氧性呼吸衰竭(AHRF)患者的插管需求,并有助于改善预后。然而,其生理机制尚不清楚。在本研究中,我们评估APP对中重度AHRF患者肺通气的影响,以更好地了解其对通气分布的影响,并预防非插管患者插管。方法:前瞻性研究于2021年1月至2022年11月在中国上海总医院重症医学科进行。研究纳入AHRF患者(氧分压[PaO2]/吸入氧浓度[FiO2] 2]/FiO2 0), APP开始后30分钟(T1), APP结束后30分钟恢复仰卧位(T2)。同时记录T0、T1、T2时SpO2、呼吸速率(RR)、FiO2、心率(HR)、ROX(脉搏血氧仪测得SpO2 /FiO2与RR之比)等临床参数。为了评估时间点对变量的影响,采用Mauchly检验进行球度检验,并采用Bonferroni事后多重比较进行重复测量方差分析。结果:10例患者入组。招募时PaO2/FiO2比值为(111.4±33.4)mmHg。APP启动后ROX显著升高{中位数(四分位数间距[IQR]): T0: 7.5 (6.0-10.1) vs. T1: 7.6 (6.4-9.3) vs. T2: 8.3 (7.2-11.0), P=0.043}。俯卧位(PP)时,RR (P=0.409)、HR (P=0.417)和SpO2/FiO2 (P=0.262)无显著变化。APP术后冠状病毒由腹侧区向背侧区转移(T0: 48.8%±6.2% vs T1: 54.8%±6.8% vs T2: 50.3%±6.1%,P=0.030)。APP术后GI明显下降(T0:中位数= 42.7%,[IQR: 38.3% ~ 47.5%] vs T1:中位数=38.2%,[IQR: 34.6% ~ 50.7%] vs T2:中位数=37.4%,[IQR: 34.2% ~ 41.4%], P=0.049)。应用APP后RVD无显著变化(P=0.794)。结论:应用APP可改善非插管AHRF患者通气分布和肺通气均匀性。中国临床试验注册号:ChiCTR2000035895。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of intensive medicine
Critical Care and Intensive Care Medicine
CiteScore
1.90
自引率
0.00%
发文量
0
审稿时长
58 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


