New drugs for acute kidney injury
引用次数: 0
Abstract
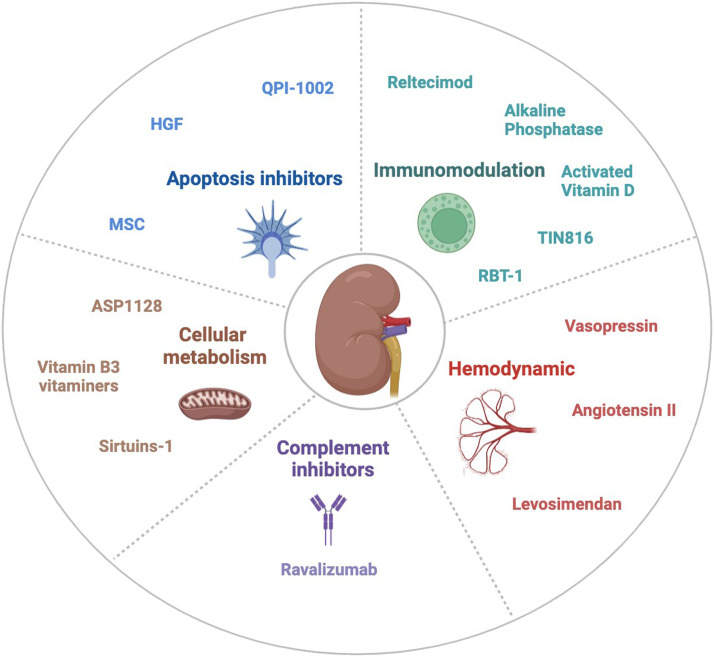
Acute kidney injury (AKI) presents a significant challenge in the management of critically ill patients, as it is associated with increased mortality, prolonged hospital stays, and increased healthcare costs. In certain conditions, such as during sepsis or after cardiac surgery, AKI is one of the most frequent complications, affecting 30%–50% of patients. Over time, even after the resolution of AKI, it can evolve into chronic kidney disease, a leading global cause of mortality, and cardiovascular complications. Despite significant improvement in the care of critically ill patients over the past two decades, the incidence of AKI remains stable, and novel approaches aiming at reducing its occurrence or improving AKI outcomes are still mostly lacking. However, recent insights into the pathophysiology of AKI within critical care settings have shed light on new pathways for both prevention and treatment, providing various new therapeutic targets aimed to mitigating kidney injury. These advancements highlight the intricate and multifaceted nature of the mechanisms underlying AKI, which could explain the challenge of identifying an effective treatment. Among these targets, modulation of the inflammatory responses and the cellular metabolism, hemodynamic regulation and enhancement of cellular repair mechanisms, have emerged as promising options. These multifaceted approaches offer renewed hope for limiting the incidence and severity of AKI in critically ill patients. Several ongoing clinical trials are evaluating the efficacy of these different strategies and we are facing an exiting time with multiple therapeutic interventions being tested to prevent or treat AKI. In this review, we aim to provide a summary of the new drugs evaluated for preventing or treating AKI in critical care and surgical settings.
治疗急性肾损伤的新药。
急性肾损伤(AKI)在重症患者的管理中提出了一个重大挑战,因为它与死亡率增加、住院时间延长和医疗费用增加有关。在某些情况下,如败血症期间或心脏手术后,AKI是最常见的并发症之一,影响30%-50%的患者。随着时间的推移,即使在AKI得到解决后,它也可能演变成慢性肾脏疾病,这是全球主要的死亡原因和心血管并发症。尽管在过去的二十年中,重症患者的护理有了显著的改善,但AKI的发病率仍然保持稳定,并且主要缺乏旨在减少其发生率或改善AKI结局的新方法。然而,最近对重症监护环境中AKI病理生理学的深入研究揭示了预防和治疗的新途径,提供了旨在减轻肾损伤的各种新的治疗靶点。这些进展突出了AKI潜在机制的复杂性和多面性,这可以解释确定有效治疗方法的挑战。在这些靶点中,炎症反应和细胞代谢的调节、血流动力学调节和细胞修复机制的增强已成为有希望的选择。这些多方面的方法为限制危重患者AKI的发生率和严重程度提供了新的希望。几个正在进行的临床试验正在评估这些不同策略的疗效,我们正面临着一个激动人心的时刻,即测试多种治疗干预措施来预防或治疗AKI。在这篇综述中,我们的目的是总结在重症监护和外科环境中预防或治疗AKI的新药。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of intensive medicine
Critical Care and Intensive Care Medicine
CiteScore
1.90
自引率
0.00%
发文量
0
审稿时长
58 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


