Autophagy activation within inflammatory microenvironment improved the therapeutic effect of MSC-Derived extracellular Vesicle in SLE
IF 11.4
1区 综合性期刊
Q1 MULTIDISCIPLINARY SCIENCES
引用次数: 0
Abstract
Introduction
Developing strategies to improve the therapeutic efficacy of mesenchymal stem cell (MSC)-derived extracellular vesicles (EVs) in autoimmune diseases have garnered increased attention.Objectives
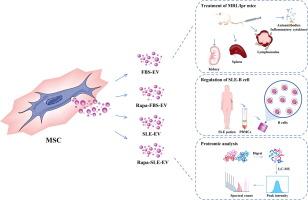
To evaluate whether rapamycin-induced autophagy within the systemic lupus erythematosus (SLE) inflammatory microenvironment (Rapa-SLE) augments the therapeutic effects of MSC-derived EVs in SLE.Methods
The therapeutic potential of the resulting EVs (Rapa-SLE-EV) was assessed in MRL/lpr mice. Rapa-SLE-EVs were compared with EVs derived from MSCs from MSCs cultured with EV-depleted fetal bovine serum (FBS-EV), EVs from MSCs cultured with rapamycin-treated FBS (Rapa-FBS-EV), and EVs exposed to SLE serum without rapamycin (SLE-EV). The autoimmune response, renal function, and pathological damage were assessed among the mouse groups. Additionally, mechanistic investigations into the role of the anti-inflammatory protein IDO1 within the EVs.Results
Interaction with the SLE inflammatory microenvironment triggered autophagy in MSCs, which was further enhanced by rapamycin treatment. Rapa-SLE-EV administration significantly ameliorated the autoimmune response and renal damage in MRL/lpr mice, outperforming other MSC-EV groups. This treatment mitigated key manifestations of SLE, including reduced autoantibody levels, as well as splenomegaly, and lymphadenopathy. Furthermore, Rapa-SLE-EV demonstrated superior suppression of plasma inflammatory cytokines, preserved renal function, mitigated pathological damage, and reduced glomerular immune complex deposition. Mechanistically, Rapa-SLE-EV exhibits exceptional inhibitory effects on SLE-B cell function, benefited by the high expression of the anti-inflammatory protein IDO1, which was confirmed to enter SLE-B cells through EVs.Conclusions
We developed a novel strategy to improve the therapeutic efficacy of MSC-EVs in SLE and confirmed that the immunomodulatory function of the MSC-EVs is enhanced through autophagic activation and interaction with the SLE serum microenvironment, a process likely benefited by the high expression of IDO1.
求助全文
约1分钟内获得全文
求助全文
来源期刊
Journal of Advanced Research
Multidisciplinary-Multidisciplinary
CiteScore
21.60
自引率
0.90%
发文量
280
审稿时长
12 weeks
期刊介绍:
Journal of Advanced Research (J. Adv. Res.) is an applied/natural sciences, peer-reviewed journal that focuses on interdisciplinary research. The journal aims to contribute to applied research and knowledge worldwide through the publication of original and high-quality research articles in the fields of Medicine, Pharmaceutical Sciences, Dentistry, Physical Therapy, Veterinary Medicine, and Basic and Biological Sciences.
The following abstracting and indexing services cover the Journal of Advanced Research: PubMed/Medline, Essential Science Indicators, Web of Science, Scopus, PubMed Central, PubMed, Science Citation Index Expanded, Directory of Open Access Journals (DOAJ), and INSPEC.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


