The Clinical Utility of Anorectal Manometry: A Review of Current Practices
引用次数: 0
Abstract
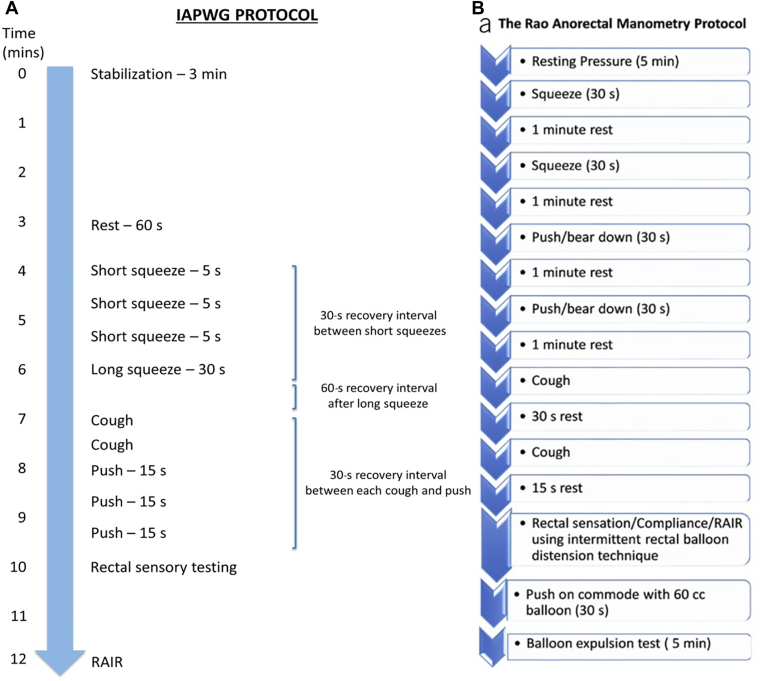
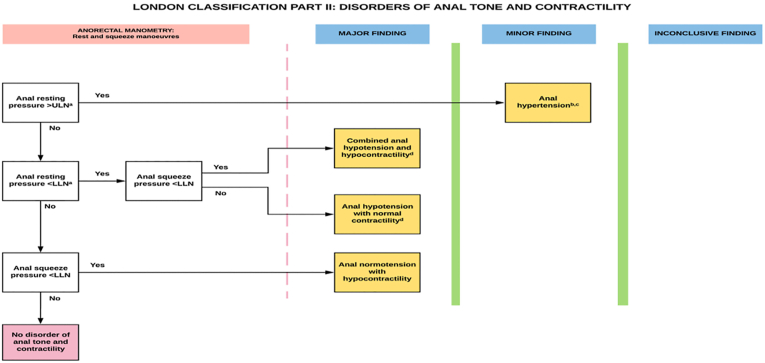
Anorectal manometry (ARM) is a diagnostic test that utilizes pressure sensors to dynamically measure intraluminal anal and rectal pressures, thus providing an objective evaluation of anorectal functional parameters (tone, contractility, and relaxation), coordination and reflex activity, and sensation. ARM is a useful test for numerous indications including for the assessment and management of functional anorectal disorders such as fecal incontinence, functional defecatory disorders, and functional anorectal pain, preoperative assessment of anorectal function, and in facilitating/assessing response to biofeedback training. In addition, while many functional anorectal disorders present with overlapping symptoms (ie constipation, anorectal pain), ARM allows delineation of more specific disease processes and may guide treatment more effectively. In recent years the development of advanced manometric methodologies such as high-resolution anorectal manometry has also led to improved spatial resolution of data acquisition, further increasing the potential for the expansion of ARM. However, despite its ability to provide detailed information on anorectal and pelvic floor muscle function and synergy as well as the endorsements of several national and international organizations, ARM is still infrequently utilized in clinical practice. The purpose of this review is to address the current clinical applications and limitations of ARM for various disorders of the lower gastrointestinal tract. In so doing, we will provide clinicians with a framework for the use of ARM in clinical practice. This review will also discuss potential barriers to widespread adoption of ARM in clinical practice and propose possible solutions to these challenges.
肛肠测压的临床应用:当前实践回顾。
肛门直肠测压(ARM)是一种诊断测试,利用压力传感器动态测量肛门和直肠腔内压力,从而提供肛门直肠功能参数(张力、收缩性和松弛性)、协调和反射活动以及感觉的客观评估。ARM是一种有用的测试,可用于评估和管理功能性肛肠疾病,如大便失禁、功能性排便障碍和功能性肛肠疼痛,术前评估肛肠功能,以及促进/评估对生物反馈训练的反应。此外,虽然许多功能性肛肠疾病存在重叠症状(如便秘、肛肠疼痛),但ARM可以描述更具体的疾病过程,并可能更有效地指导治疗。近年来,高分辨率肛门直肠测压等先进测压方法的发展也提高了数据采集的空间分辨率,进一步增加了ARM扩展的潜力。然而,尽管ARM能够提供肛门直肠和盆底肌肉功能和协同作用的详细信息,并且得到了几个国家和国际组织的认可,但在临床实践中仍然很少使用ARM。本综述的目的是讨论ARM在各种下胃肠道疾病中的临床应用和局限性。这样,我们将为临床医生在临床实践中使用ARM提供一个框架。本综述还将讨论在临床实践中广泛采用ARM的潜在障碍,并提出应对这些挑战的可能解决方案。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


