A unique case of extranodal marginal zone lymphoma with synchronous pulmonary and dermatologic manifestations
IF 0.7
Q4 RESPIRATORY SYSTEM
引用次数: 0
Abstract
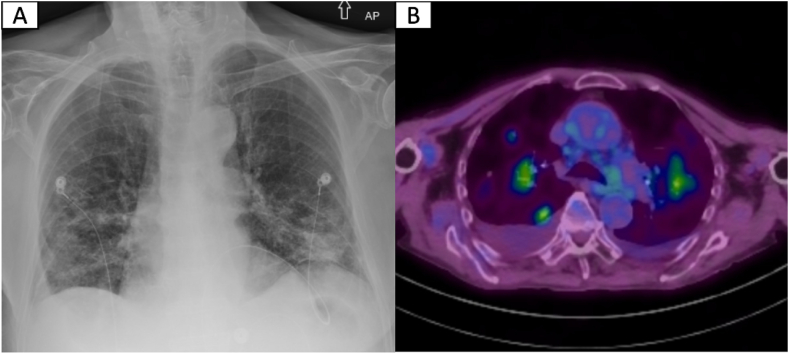
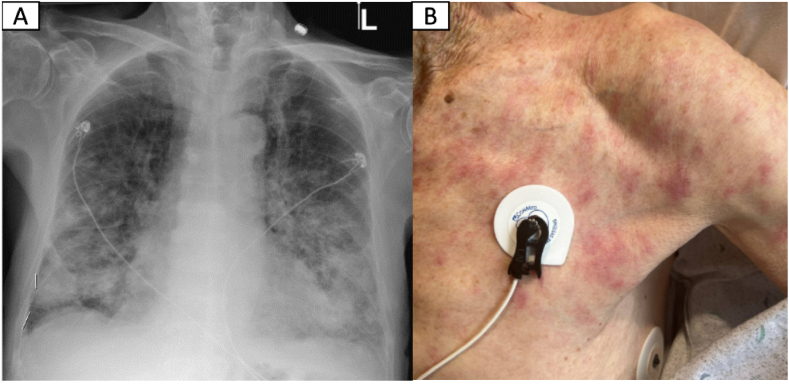
An 89-year-old male with a medical history of non-ischemic cardiomyopathy was initially admitted with acute hypoxic respiratory failure attributed to heart failure exacerbation. Aside from progressive dyspnea, a non-pruritic, non-painful rash and constitutional symptoms were reported. Initial work-up was remarkable for normocytic anemia, lymphopenia, mild hypercalcemia, and elevated inflammatory markers. Despite aggressive diuresis, his respiratory distress worsened requiring up-titration of supplemental oxygen (6–8L/min). Subsequent chest CT showed diffuse, ill-defined areas of consolidation and ground-glass opacities (GGOs) with areas of solid and ground-glass nodularity. Rheumatologic work-up was remarkable for mildly elevated ANA titer of 1:60, and positive anti-centromere antibody of 1.8 AI (normal range 0–0.9 AI). Infectious work-up was negative. Due to high oxygen requirements, tissue sampling was obtained by skin biopsy instead of bronchoscopy. After biopsy testing, prednisone 60 mg was started with posterior clinical and radiographic improvement. Biopsy results revealed cutaneous MZL. Follow-up PET scan showed persistent but improved diffuse GGOs and nodular opacities. Given the clinical presentation, imaging and skin biopsy results, the diagnosis was compatible with EMZL with synchronous pulmonary and skin manifestations. Empiric treatment with Rituximab and steroid taper was planned. At 6-month follow-up, the patient reported clinical and respiratory improvement.

结外边缘区淋巴瘤的独特病例,伴有肺部和皮肤的同步表现。
89岁男性,既往有非缺血性心肌病病史,因心力衰竭加重导致急性缺氧性呼吸衰竭入院。除了进行性呼吸困难外,还报告了非瘙痒性,非疼痛性皮疹和体质症状。最初的检查显示正常细胞性贫血、淋巴细胞减少、轻度高钙血症和炎症标志物升高。尽管积极利尿,他的呼吸窘迫恶化,需要增加补氧滴定(6-8L/min)。随后的胸部CT显示弥漫性,不明确的实变区和磨玻璃影(GGOs),伴实性和磨玻璃结节。风湿病检查中ANA滴度轻度升高1:60,抗着丝粒抗体阳性1.8 AI(正常范围0-0.9 AI)。感染检查呈阴性。由于高氧需求,组织取样是通过皮肤活检而不是支气管镜。活检检查后,在临床和影像学改善后开始使用强的松60mg。活检结果显示皮肤MZL。随访PET扫描显示持续但改善的弥漫性ggo和结节性混浊。结合临床表现、影像学及皮肤活检结果,诊断符合EMZL,肺及皮肤同步表现。计划使用利妥昔单抗和类固醇减量治疗。在6个月的随访中,患者报告临床和呼吸改善。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Respiratory Medicine Case Reports
RESPIRATORY SYSTEM-
CiteScore
2.10
自引率
0.00%
发文量
213
审稿时长
87 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


