Neoadjuvant nivolumab and chemotherapy in early estrogen receptor-positive breast cancer: a randomized phase 3 trial
IF 58.7
1区 医学
Q1 BIOCHEMISTRY & MOLECULAR BIOLOGY
引用次数: 0
Abstract
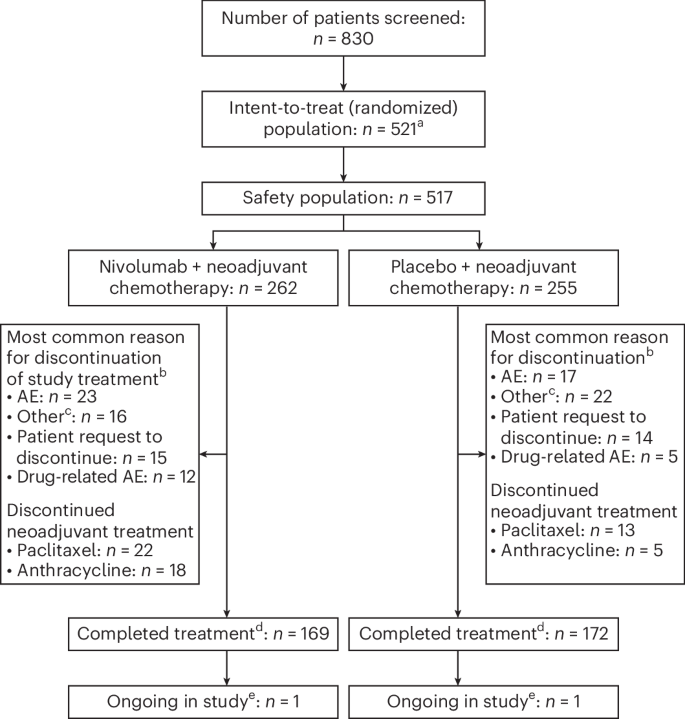
Patients with estrogen receptor-positive (ER+), human epidermal growth factor receptor 2-negative (HER2−) primary breast cancer (BC) have low pathological complete response (pCR) rates with neoadjuvant chemotherapy. A subset of ER+/HER2− BC contains dense lymphocytic infiltration. We hypothesized that addition of an anti-programmed death 1 agent may increase pCR rates in this BC subtype. We conducted a randomized, multicenter, double-blind phase 3 trial to investigate the benefit of adding nivolumab to neoadjuvant chemotherapy in patients with newly diagnosed, high-risk, grade 3 or 2 (ER 1 to ≤10%) ER+/HER2− primary BC. In total, 510 patients were randomized to receive anthracycline and taxane-based chemotherapy with either intravenous nivolumab or placebo. The primary endpoint of pCR was significantly higher in the nivolumab arm compared with placebo (24.5% versus 13.8%; P = 0.0021), with greater benefit observed in patients with programmed death ligand 1-positive tumors (VENTANA SP142 ≥1%: 44.3% versus 20.2% respectively). There were no new safety signals identified. Of the five deaths that occurred in the nivolumab arm, two were related to study drug toxicity; no deaths occurred in the placebo arm. Adding nivolumab to neoadjuvant chemotherapy significantly increased pCR rates in high-risk, early-stage ER+/HER2− BC, particularly among patients with higher stromal tumor-infiltrating lymphocyte levels or programmed death ligand 1 expression, suggesting a new treatment paradigm that emphasizes the role of immunotherapy and T cell immunosurveillance in luminal disease. Clinical trials.gov identifier: NCT04109066 In the CheckMate 7FL trial, neoadjuvant nivolumab and chemotherapy in patients with newly diagnosed, high-risk estrogen receptor-positive breast cancer led to an increased pathological complete response rate compared with neoadjuvant chemotherapy alone, and this increase was associated with immune-related biomarkers and estrogen receptor expression.

早期雌激素受体阳性乳腺癌的新辅助纳武单抗和化疗:一项随机3期试验
雌激素受体阳性(ER+)、人表皮生长因子受体2阴性(HER2−)原发性乳腺癌(BC)患者在新辅助化疗中病理完全缓解(pCR)率较低。ER+/HER2−BC的一个亚群含有密集的淋巴细胞浸润。我们假设添加一种抗程序性死亡1剂可能会增加这种BC亚型的pCR率。我们进行了一项随机、多中心、双盲的3期试验,以研究在新诊断、高风险、3级或2级(ER 1至≤10%)ER+/HER2 -原发性BC患者中加入纳武单抗的新辅助化疗的益处。总共有510名患者随机接受蒽环类和紫杉烷类化疗,静脉注射纳武单抗或安慰剂。纳武单抗组pCR的主要终点明显高于安慰剂组(24.5% vs 13.8%;P = 0.0021),程序性死亡配体1阳性肿瘤患者获益更大(VENTANA SP142≥1%:分别为44.3%和20.2%)。没有发现新的安全信号。在纳武单抗组发生的5例死亡中,2例与研究药物毒性有关;在安慰剂组中没有发生死亡。在新辅助化疗中加入纳鲁单抗可显著提高高危、早期ER+/HER2 - BC的pCR率,特别是在基质肿瘤浸润性淋巴细胞水平较高或程序性死亡配体1表达较高的患者中,提示一种新的治疗模式,强调免疫治疗和T细胞免疫监测在管腔疾病中的作用。临床试验。gov标识符:NCT04109066
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Nature Medicine
医学-生化与分子生物学
CiteScore
100.90
自引率
0.70%
发文量
525
审稿时长
1 months
期刊介绍:
Nature Medicine is a monthly journal publishing original peer-reviewed research in all areas of medicine. The publication focuses on originality, timeliness, interdisciplinary interest, and the impact on improving human health. In addition to research articles, Nature Medicine also publishes commissioned content such as News, Reviews, and Perspectives. This content aims to provide context for the latest advances in translational and clinical research, reaching a wide audience of M.D. and Ph.D. readers. All editorial decisions for the journal are made by a team of full-time professional editors.
Nature Medicine consider all types of clinical research, including:
-Case-reports and small case series
-Clinical trials, whether phase 1, 2, 3 or 4
-Observational studies
-Meta-analyses
-Biomarker studies
-Public and global health studies
Nature Medicine is also committed to facilitating communication between translational and clinical researchers. As such, we consider “hybrid” studies with preclinical and translational findings reported alongside data from clinical studies.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


