Alcohol Relapse After Liver Transplantation: Risk Factors, Outcomes, and a Comparison of Risk Stratification Models
引用次数: 0
Abstract
Background and Aims
Alcohol-related liver disease is a leading cause of liver transplantation (LT) in the United States; however, alcohol relapse remains a risk, and real-world assessment of relapse prediction scores is lacking. The primary aim of this study was to assess risk factors for alcohol relapse and compare effectiveness of pre-existing risk scores (e.g., Sustained Alcohol Use Post-Liver Transplant (SALT) and Harmful Alcohol Use Post-Liver Transplant (HALT) scores).
Methods
This was a retrospective chart review of 69 adults who underwent LT for alcohol-related liver disease at Duke University Hospital from January 1, 2018, to January 1, 2021. Outcome variables included relapse post-LT, severity of relapse, and graft dysfunction.
Results
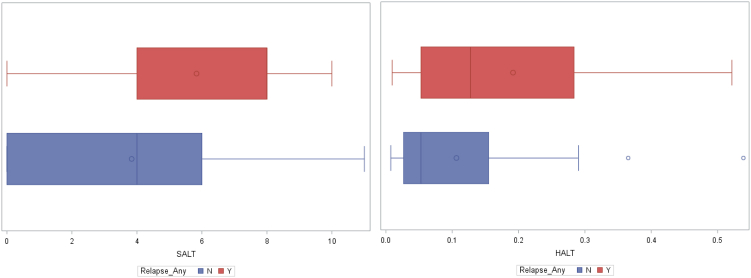
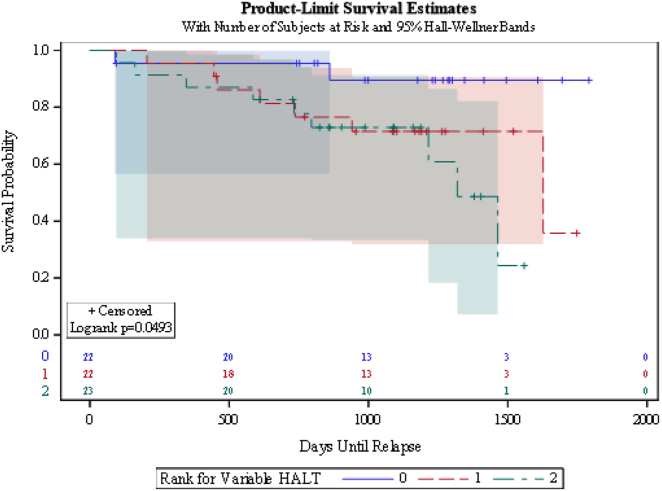
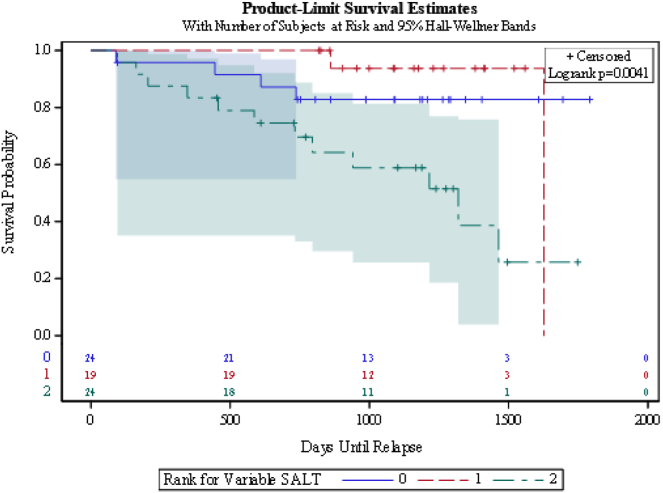
Sixty-seven patients with a median follow-up time of 43 months were included. Eighteen (27%) experienced alcohol relapse. Of those, 16 (89%) had heavy alcohol use and 3 of those patients (17%) experienced graft dysfunction. Factors significantly associated with relapse included younger age, prior relapse, significant psychiatric comorbidities, alcohol use after cirrhosis diagnosis, shorter abstinence before LT listing, and prior alcohol treatment program. When applying SALT and HALT scores, the area under the curve was 0.69 (95% confidence interval 0.53–0.85) and 0.66 (95% confidence interval 0.50–0.81), respectively.
Conclusion
In our cohort, heavy alcohol use before transplantation and legal issues did not predict relapse, which are common components of prediction scores. Less than 5% of patients had graft dysfunction due to relapse, suggesting good graft outcomes. While the HALT and SALT scores were validated in our cohort, our finding of additional significant predictors of relapse, in addition to previously reported risk factors providing protective effect, suggests opportunity for further optimization of prediction scores.
肝移植后酒精复发:危险因素、结果和风险分层模型的比较
背景和目的:在美国,酒精相关肝病是导致肝移植(LT)的主要原因之一;然而,酒精复发仍然是一种风险,而且缺乏对复发预测评分的真实世界评估。本研究的主要目的是评估酒精复发的风险因素,并比较已有风险评分(如肝移植后持续酒精使用评分(SALT)和肝移植后有害酒精使用评分(HALT))的有效性:这是一项回顾性病历审查,对象是2018年1月1日至2021年1月1日期间在杜克大学医院接受LT治疗酒精相关肝病的69名成人。结果变量包括LT后复发、复发严重程度和移植物功能障碍:共纳入 67 名患者,中位随访时间为 43 个月。18例(27%)患者复发酒精中毒。其中 16 人(89%)酗酒严重,3 人(17%)出现移植物功能障碍。与复发密切相关的因素包括:年龄较小、曾有复发、严重的精神并发症、肝硬化确诊后饮酒、LT 患者上市前戒酒时间较短、曾接受过酒精治疗项目。在应用SALT和HALT评分时,曲线下面积分别为0.69(95%置信区间0.53-0.85)和0.66(95%置信区间0.50-0.81):在我们的队列中,移植前大量饮酒和法律问题并不能预测复发,而这是预测评分的常见组成部分。不到5%的患者因复发导致移植功能障碍,这表明移植结果良好。虽然HALT和SALT评分在我们的队列中得到了验证,但除了之前报道的具有保护作用的风险因素外,我们还发现了其他重要的复发预测因素,这为进一步优化预测评分提供了机会。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


