Tuberculous meningitis-related ischemic stroke: A retrospective study from a tertiary care hospital
IF 2
Q3 INFECTIOUS DISEASES
Journal of Clinical Tuberculosis and Other Mycobacterial Diseases
Pub Date : 2025-02-01
DOI:10.1016/j.jctube.2024.100508
引用次数: 0
Abstract
Background
Patients with tuberculous meningitis (TBM) are at high risk of ischemic stroke, and stroke is a poor prognosticator of TBM. However, reports regarding the predictors of stroke in TBM patients are scanty. The aim of this study was to investigate the clinical characteristics and predictors of tuberculous meningitis-related ischemic stroke (TBMRIS).
Methods
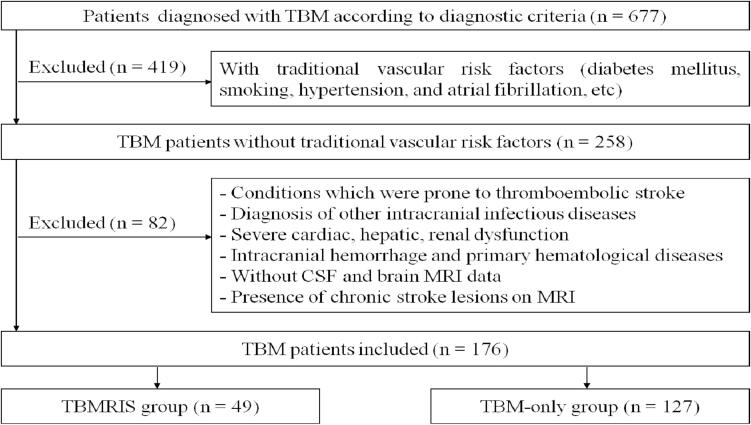
This retrospective study was conducted among TBM patients without traditional vascular risk factors from a tertiary care hospital between January 2017 and November 2022. Patients were divided into TBMRIS group and TBM-only group according to presence of stroke. Clinical, laboratory and radiological variables were compared between the two groups. Predictors of stroke were identified using binary logistic regression analysis.
Results
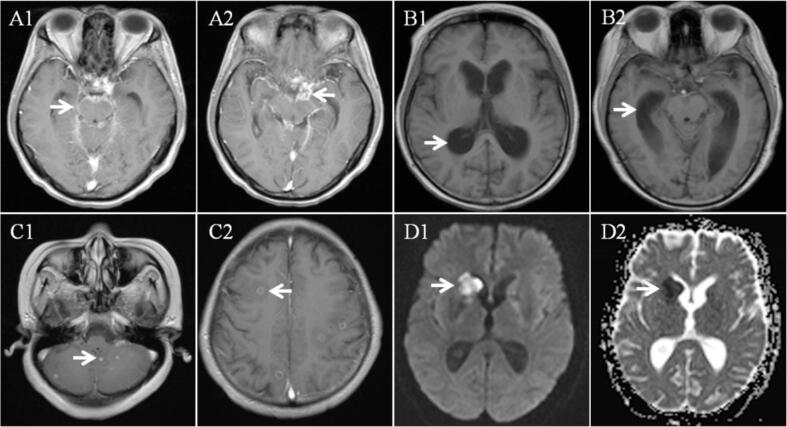
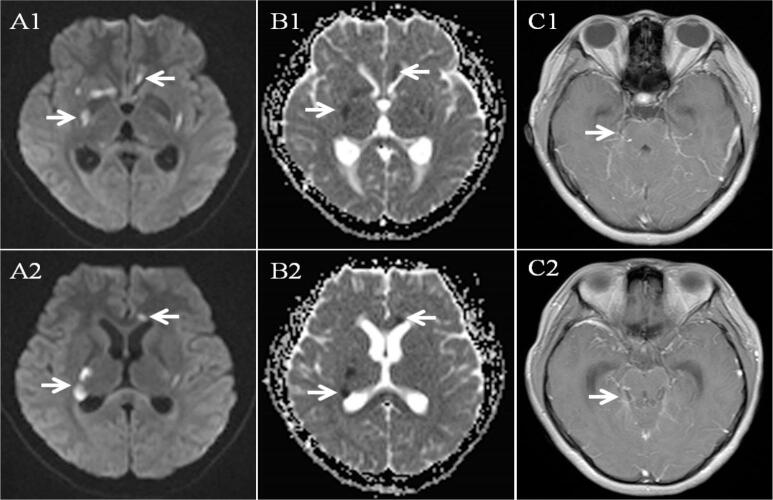
A total of 176 TBM patients were included in the study. Forty-nine patients with stroke were classified as TBMRIS group and 127 patients without stroke were classified as TBM-only group. In TBMRIS group, 41 (83.7 %) patients experienced stroke within 3 months after the onset of meningitis symptoms and 10 (20.4 %) patients presented silent stroke. Stroke occurred in basal ganglia in 57.1 % of patients. About 73.5 % of patients showed multiple stroke lesions and 38.8 % of patients had stroke involving multiple vascular territories. There were significant differences in focal neurological deficit, stage of meningitis, short-term outcome, serum sodium, cerebrospinal fluid (CSF) white cell count, CSF adenosine deaminase (ADA), CSF protein, leptomeningeal enhancement, tuberculoma between TBMRIS group and TBM-only group. Binary logistic regression analysis revealed that focal neurological deficit, CSF white cell count and leptomeningeal enhancement were the independent risk factors for stroke, and tuberculoma was negatively correlated with stroke.
Conclusion
Most of TBMRIS develop within 3 months after the onset of meningitis symptoms and basal ganglia is the most frequent site. Multiple stroke lesions and involvement of multiple vascular territories are commonly observed. Focal neurological deficit, CSF white cell count and leptomeningeal enhancement are the predictors of stroke in patients with TBM.
结核性脑膜炎相关缺血性脑卒中:来自三级医院的回顾性研究。
背景:结核性脑膜炎(TBM)患者发生缺血性卒中的风险较高,卒中是TBM的不良预后因素。然而,关于TBM患者中风预测因素的报道很少。本研究的目的是探讨结核性脑膜炎相关缺血性脑卒中(TBMRIS)的临床特征和预测因素。方法:回顾性研究于2017年1月至2022年11月在某三级医院无传统血管危险因素的TBM患者。根据脑卒中情况将患者分为脑mri组和单纯脑mri组。比较两组患者的临床、实验室及影像学指标。采用二元逻辑回归分析确定脑卒中的预测因素。结果:共纳入176例TBM患者。49例脑卒中患者被分为tbmri组,127例非脑卒中患者被分为tbm组。TBMRIS组中,41例(83.7%)患者在出现脑膜炎症状后3个月内发生脑卒中,10例(20.4%)患者出现无症状脑卒中。57.1%的患者发生在基底节区。约73.5%的患者出现多发性脑卒中病变,38.8%的患者卒中累及多血管区域。在局灶性神经功能缺损、脑膜炎分期、短期预后、血清钠、脑脊液白细胞计数、脑脊液腺苷脱氨酶(ADA)、脑脊液蛋白、脑脊液轻脑膜增强、结核瘤等方面,TBMRIS组与单纯tms组差异均有统计学意义。二元logistic回归分析显示局灶性神经功能缺损、脑脊液白细胞计数和脑脊膜轻脑膜增强是脑卒中的独立危险因素,而结核瘤与脑卒中呈负相关。结论:TBMRIS多在出现脑膜炎症状后3个月内发病,基底节区是最常见的发病部位。多发脑卒中病变和多血管区域受累是常见的。局灶性神经功能缺损、脑脊液白细胞计数和脑脊膜轻脑膜增强是TBM患者脑卒中的预测因子。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Clinical Tuberculosis and Other Mycobacterial Diseases
Medicine-Pulmonary and Respiratory Medicine
CiteScore
4.00
自引率
5.00%
发文量
44
审稿时长
30 weeks
期刊介绍:
Journal of Clinical Tuberculosis and Mycobacterial Diseases aims to provide a forum for clinically relevant articles on all aspects of tuberculosis and other mycobacterial infections, including (but not limited to) epidemiology, clinical investigation, transmission, diagnosis, treatment, drug-resistance and public policy, and encourages the submission of clinical studies, thematic reviews and case reports. Journal of Clinical Tuberculosis and Mycobacterial Diseases is an Open Access publication.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


