Effects of conditional cash transfers on tuberculosis incidence and mortality according to race, ethnicity and socioeconomic factors in the 100 Million Brazilian Cohort
IF 50
1区 医学
Q1 BIOCHEMISTRY & MOLECULAR BIOLOGY
引用次数: 0
Abstract
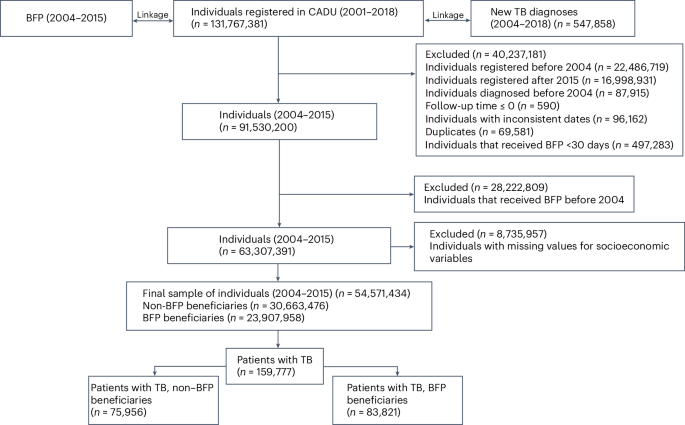
Conditional cash transfer (CCT) programs have been implemented globally to alleviate poverty. Although tuberculosis (TB) is closely linked to poverty, the effects of CCT on TB outcomes among populations facing social and economic vulnerabilities remain uncertain. Here we estimated the associations between participation in the world’s largest CCT program, the Brazilian Bolsa Família Program (BFP), and the reduction of TB incidence, mortality and case-fatality rates using the nationwide 100 Million Brazilian Cohort between 2004 and 2015. We also evaluated these relationships according to race, ethnicity, wealth levels, sex and age. Exposure to the BFP was associated with a large reduction in TB incidence (adjusted rate ratio (aRR): 0.59; 95% confidence interval (CI): 0.58–0.60) and mortality (aRR: 0.69; 95% CI: 0.65–0.73). The strongest BFP association was observed in individuals of Indigenous ethnicity both for TB incidence (aRR: 0.37; 95% CI: 0.32–0.42) and mortality (aRR: 0.35; 95% CI: 0.20–0.62), and in individuals of Black and Pardo ethnicity (incidence—aRR: 0.58; 95% CI: 0.57–0.59; mortality—aRR: 0.69; 95% CI: 0.64–0.73). BFP associations were considerably stronger among individuals living in extreme poverty both for TB incidence (aRR: 0.49; 95% CI: 0.49–0.50) and mortality (aRR: 0.60; 95% CI: 0.55–0.65). CCT can strongly reduce TB incidence and mortality in individuals living in extreme poverty, and of Indigenous, Black and Pardo ethnicity, and could significantly contribute to achieving the End TB Strategy targets and TB-related Sustainable Development Goals. Participation in Brazil’s Bolsa Familia Program, one of the largest conditional cash transfer programs in the world, was associated with large reductions in tuberculosis incidence and mortality among Indigenous people, individuals of Black and Pardo ethnicity and those living in extreme poverty.

有条件现金转移对1亿巴西队列中按种族、民族和社会经济因素划分的结核病发病率和死亡率的影响
有条件现金转移支付(CCT)项目已在全球范围内实施,以减轻贫困。尽管结核病与贫困密切相关,但有条件现金援助对面临社会和经济脆弱性人群的结核病结果的影响仍然不确定。在这里,我们利用2004年至2015年全国1亿巴西队列,估计了参与世界上最大的有条件现金转移支付项目巴西Bolsa Família项目(BFP)与结核病发病率、死亡率和病死率降低之间的关系。我们还根据种族、民族、财富水平、性别和年龄评估了这些关系。暴露于BFP与结核病发病率的大幅降低相关(调整比率(aRR): 0.59;95%置信区间(CI): 0.58-0.60)和死亡率(aRR: 0.69;95% ci: 0.65-0.73)。在土著民族个体中观察到最强的BFP与结核病发病率的关联(aRR: 0.37;95% CI: 0.32-0.42)和死亡率(aRR: 0.35;95% CI: 0.20-0.62),黑人和帕尔多族个体(发病率- arr: 0.58;95% ci: 0.57-0.59;mortality-aRR: 0.69;95% ci: 0.64-0.73)。在极度贫困人群中,BFP与结核病发病率的关联明显更强(aRR: 0.49;95% CI: 0.49-0.50)和死亡率(aRR: 0.60;95% ci: 0.55-0.65)。有条件现金资助可以大大降低极端贫困人群以及土著、黑人和帕尔多族人群的结核病发病率和死亡率,并可为实现《终止结核病战略》的具体目标和与结核病相关的可持续发展目标作出重大贡献。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Nature Medicine
医学-生化与分子生物学
CiteScore
100.90
自引率
0.70%
发文量
525
审稿时长
1 months
期刊介绍:
Nature Medicine is a monthly journal publishing original peer-reviewed research in all areas of medicine. The publication focuses on originality, timeliness, interdisciplinary interest, and the impact on improving human health. In addition to research articles, Nature Medicine also publishes commissioned content such as News, Reviews, and Perspectives. This content aims to provide context for the latest advances in translational and clinical research, reaching a wide audience of M.D. and Ph.D. readers. All editorial decisions for the journal are made by a team of full-time professional editors.
Nature Medicine consider all types of clinical research, including:
-Case-reports and small case series
-Clinical trials, whether phase 1, 2, 3 or 4
-Observational studies
-Meta-analyses
-Biomarker studies
-Public and global health studies
Nature Medicine is also committed to facilitating communication between translational and clinical researchers. As such, we consider “hybrid” studies with preclinical and translational findings reported alongside data from clinical studies.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


