Empagliflozin in acute myocardial infarction in patients with and without type 2 diabetes: A pre‐specified analysis of the EMPACT‐MI trial
IF 16.9
1区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
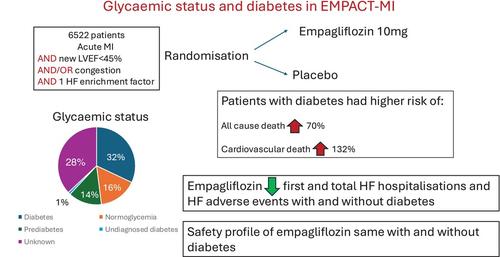
AimsIn the EMPACT‐MI trial, empagliflozin reduced heart failure (HF) hospitalizations but not mortality in acute myocardial infarction (MI). Contemporary reports of clinical event rates with and without type 2 diabetes mellitus (T2DM) in acute MI trials are sparse. The treatment effect of empagliflozin in those with and without T2DM in acute MI is unknown.Methods and resultsA total of 6522 patients with acute MI with newly reduced left ventricular ejection fraction (LVEF) to <45%, congestion, or both, were randomized to empagliflozin 10 mg or placebo. The primary endpoint was time to first HF hospitalization or all‐cause death. Rates of endpoints with and without T2DM and the efficacy and safety of empagliflozin according to T2DM status were assessed. Overall, 32% had T2DM; 14% had pre‐diabetes; 16% were normoglycaemic; 38% had unknown glycaemic status. Patients with T2DM, compared to those without T2DM, were at higher risk of time to first HF hospitalization or all‐cause death (hazard ratio [HR] 1.44; 95% confidence interval [CI] 1.06–1.95) and all‐cause death (HR 1.70; 95% CI 1.13–2.56). T2DM did not confer a higher risk of first HF hospitalization (HR 1.22, 95% CI 0.82–1.83). Empagliflozin reduced first and total HF hospitalizations, but not all‐cause mortality, regardless of presence or absence of T2DM. The safety profile of empagliflozin was the same with and without T2DM.ConclusionPatients with acute MI, LVEF <45% and/or congestion who had T2DM were at a higher risk of mortality than those without T2DM. Empagliflozin reduced first and total HF hospitalizations regardless of the presence or absence of T2DM.
求助全文
约1分钟内获得全文
求助全文
来源期刊

European Journal of Heart Failure
医学-心血管系统
CiteScore
27.30
自引率
11.50%
发文量
365
审稿时长
1 months
期刊介绍:
European Journal of Heart Failure is an international journal dedicated to advancing knowledge in the field of heart failure management. The journal publishes reviews and editorials aimed at improving understanding, prevention, investigation, and treatment of heart failure. It covers various disciplines such as molecular and cellular biology, pathology, physiology, electrophysiology, pharmacology, clinical sciences, social sciences, and population sciences. The journal welcomes submissions of manuscripts on basic, clinical, and population sciences, as well as original contributions on nursing, care of the elderly, primary care, health economics, and other related specialist fields. It is published monthly and has a readership that includes cardiologists, emergency room physicians, intensivists, internists, general physicians, cardiac nurses, diabetologists, epidemiologists, basic scientists focusing on cardiovascular research, and those working in rehabilitation. The journal is abstracted and indexed in various databases such as Academic Search, Embase, MEDLINE/PubMed, and Science Citation Index.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


