AI model using CT-based imaging biomarkers to predict hepatocellular carcinoma in patients with chronic hepatitis B
IF 26.8
1区 医学
Q1 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
Abstract
Background & aims
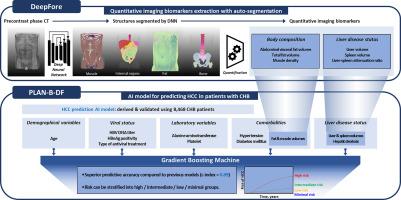
Various hepatocellular carcinoma (HCC) prediction models have been proposed for patients with chronic hepatitis B (CHB) using clinical variables. We aimed to develop an artificial intelligence (AI)-based HCC prediction model by incorporating imaging biomarkers derived from abdominal computed tomography (CT) images along with clinical variables.Methods
An AI prediction model employing a gradient-boosting machine algorithm was developed utilizing imaging biomarkers extracted by DeepFore, a deep learning-based CT auto-segmentation software. The derivation cohort (n=5,585) was randomly divided into the training and internal validation sets at a 3:1 ratio. The external validation cohort included 2,883 patients. Six imaging biomarkers (i.e., abdominal visceral fat–total fat volume ratio, total fat–trunk volume ratio, spleen, and liver volume; liver–spleen Hounsfield unit [HU] ratio; and muscle HU) and eight clinical variables were selected as the main variables of our model, PLAN-B-DF.Results
In the internal validation set (median follow-up duration=7.4 years), PLAN-B-DF demonstrated an excellent predictive performance with a c-index of 0.91 and good calibration function (P=0.78 by the Hosmer-Lemeshow test). In the external validation cohort (median follow-up duration=4.6 years), PLAN-B-DF showed a significantly better discrimination function compared to previous models including PLAN-B, PAGE-B, modified PAGE-B, and CU-HCC (c-index, 0.89 vs. 0.65—0.78; all P<0.001) and maintained a good calibration function (P=0.42 by the Hosmer-Lemeshow test). When patients were classified into four groups according to the risk probability calculated by PLAN-B-DF, the 10-year cumulative HCC incidence was 0.0%, 0.4%, 16.0%, and 46.2% in the minimal-, low-, intermediate-, and high-risk groups, respectively.Conclusion
This AI prediction model, integrating deep learning-based auto-segmentation of CT images, offers improved performance in predicting HCC risk among patients with CHB compared to previous models.Impact and implications
The AI-driven HCC prediction model (PLAN-B-DF), employing an automated CT segmentation algorithm, demonstrates a significant improvement in predictive accuracy and risk stratification among patients with CHB. Using a gradient-boosting algorithm and CT metrics such as visceral fat volume and myosteatosis, PLAN-B-DF outperforms previous models based solely on clinical and demographic data. This model not only shows a higher c-index compared to previous models, but also effectively classifies CHB patients into different risk groups. This model uses machine learning to analyze the complex relationships among various risk factors contributing to HCC occurrence, thereby offering more personalized surveillance for CHB patients.
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Hepatology
医学-胃肠肝病学
CiteScore
46.10
自引率
4.30%
发文量
2325
审稿时长
30 days
期刊介绍:
The Journal of Hepatology is the official publication of the European Association for the Study of the Liver (EASL). It is dedicated to presenting clinical and basic research in the field of hepatology through original papers, reviews, case reports, and letters to the Editor. The Journal is published in English and may consider supplements that pass an editorial review.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


