Association between body mass index and clinical outcomes in patients with acute myocardial infarction and reduced systolic function: Analysis of PARADISE-MI trial data
Abstract
Aims
The relationship between body mass index (BMI) and clinical outcomes in patients with cardiovascular disease, including acute heart failure (AHF) and acute myocardial infarction (AMI), remains debated. This study investigates the association between BMI and clinical outcomes within the PARADISE-MI cohort, while also evaluating the impact of angiotensin receptor–neprilysin inhibitor (ARNI) versus angiotensin-converting enzyme inhibitor (ACE-I) treatment on this relationship.
Methods and results
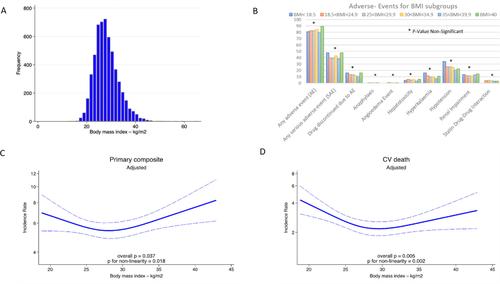
The analysis included 5589 patients from the PARADISE-MI study with available baseline BMI data. The cohort comprised patients with AMI and pulmonary congestion and/or left ventricular ejection fraction ≤40%. Patients were categorized into six World Health Organization BMI subgroups. The primary outcome of interest was the composite endpoint of cardiovascular death, heart failure (HF)-associated hospitalization, and outpatient symptomatic HF episodes. The mean baseline BMI of the cohort was 28.1 ± 5.0 kg/m2. The lowest rate of the primary composite endpoint (6.2/100 patient-years) was observed in overweight patients (BMI 25–29.9 kg/m2), while the highest rates were found in the lowest and highest BMI subgroups (8.4/100 patient-years for BMI <18.5 kg/m2 and 9.7/100 patient-years for BMI >40 kg/m2). There was no significant interaction between BMI and the treatment effect of ARNI versus ACE-I on the primary composite outcome (p = 0.73). Additionally, no significant differences in the incidence of adverse events or serious adverse events were noted across the BMI subgroups.
Conclusions
In AMI with AHF patients, the relationship between BMI and the primary composite outcome is non-linear, with the lowest event rates observed in overweight individuals. Outcomes and safety profiles for ARNI and ACE-I treatments were similar across BMI subgroups.


 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


