All-cause and cause-specific mortality in patients with chronic hepatitis B and concurrent steatotic liver disease
IF 26.8
1区 医学
Q1 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
Abstract
Background & Aims
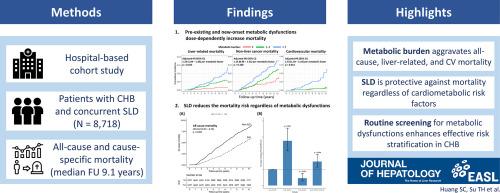
Steatotic liver disease (SLD) is prevalent among patients with chronic hepatitis B (CHB). However, the effects of metabolic dysfunction–associated SLD (MASLD) on the long-term survival of such patients remain unknown. Accordingly, this study investigated the mortality risks in patients with CHB and concurrent SLD.Methods
Consecutive patients with CHB and concurrent SLD were retrospectively recruited at National Taiwan University Hospital. MASLD was defined by the presence of cardiometabolic risk factors (CMRF). The cumulative incidences of all-cause and cause-specific mortality were compared.Results
A total of 8,718 patients with CHB and concurrent SLD were included from 2006 to 2021. At baseline, the MASLD group (n=6,562) was older and had a lower proportion of hepatitis B e antigen positivity and lower hepatitis B virus DNA levels compared with the non-MASLD group (n=2,156). After a median follow-up period of 9.1 years, the MASLD group exhibited a higher risk of all-cause mortality compared with the non-MASLD group (adjusted hazard ratio [aHR]: 1.79, 95% confidence interval [CI]: 1.24–2.58, p=0.002). Furthermore, cumulative CMRF dose-dependently elevated the risks of all-cause, liver-related, and cardiovascular mortality (all p<0.05). During the follow-up period, new-onset diabetes mellitus, hypertension, and significant weight gain further increased the risks of all-cause and liver-related mortality (all p<0.05). However, patients with SLD had a lower mortality risk than non-SLD patients after propensity score matching (HR: 0.62, 95% CI: 0.53 – 0.74, p<0.001).Conclusions
Among patients with CHB and SLD, metabolic burden dose-dependently increases the all-cause, liver-related, and cardiovascular mortality risks. Patients with SLD have a lower mortality risk than those without SLD. Identifying these metabolic dysfunctions is crucial for stratifying the level of risk in daily care.Impact and Implications
Concurrent steatotic liver disease (SLD) is prevalent among patients with chronic hepatitis B (CHB); however, the effects of the associated cardiometabolic risk factors on all-cause and cause-specific mortality remain unknown. This study demonstrated that cumulative metabolic burden dose-dependently increased the risks of all-cause, liver-related, and cardiovascular mortality in patients with CHB and SLD. Moreover, new-onset diabetes mellitus, hypertension, and weight gain during the follow-up period further exacerbated these risks. However, patients with SLD had a lower risk of mortality than those without SLD. Thus, routine screening and monitoring of metabolic dysfunctions constitute a key element of daily care for patients with CHB.
慢性乙型肝炎并发脂肪肝患者的全因和特定原因死亡率
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Hepatology
医学-胃肠肝病学
CiteScore
46.10
自引率
4.30%
发文量
2325
审稿时长
30 days
期刊介绍:
The Journal of Hepatology is the official publication of the European Association for the Study of the Liver (EASL). It is dedicated to presenting clinical and basic research in the field of hepatology through original papers, reviews, case reports, and letters to the Editor. The Journal is published in English and may consider supplements that pass an editorial review.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


